
Thoracoscopic transareolar approach for primary spontaneous pneumothorax in young male patients
Introduction
Most patients with primary spontaneous pneumothorax (PSP) are treated via thoracoscopic surgery. However, the number of ports used during thoracoscopic surgery (i.e., uni- or multi-port) varies among each institution. Although the multiportal approach was commonly used previously, uniportal approach has increasingly been used in the last decade (1-8). The uniportal approach involves making a 2–3-cm-long single skin incision along the lateral axillary line, which leads to less postoperative pain and higher cosmetic satisfaction than the multiportal approach. In our previous study, we compared the efficacy of the uni- and multi-portal approaches for thoracoscopic bullectomy for the treatment of PSP (8).
The uniportal approach is not commonly used, despite its less invasive nature; this may be because surgical instrument maneuvering is markedly different between the uni- and multiportal approaches. In the uniportal approach, several instruments, including forceps, a stapler, and a thoracoscope, are simultaneously inserted through a single skin incision, which may be difficult to maneuver for inexperienced surgeons.
Operation
To defeat the difficulty associated with the insertion of multiple instruments, we developed the thoracoscopic “transareolar” approach for bullectomy in September 2017 as an alternative to the minimally invasive approach (9). The transareolar approach was performed with the patients under general anesthesia using single-lung ventilation in the lateral decubitus position (Video 1). The areola was put on the level of the fourth intercostal space by moving the patient’s arm. We made a 2-cm arc incision for applying staples on the upper edge of the areola, as well as a 5-mm arc incision for the insertion of forceps on the lower edge of the areola. Both incisions were created at the level of the fourth intercostal space. The 2-cm incision was covered with an XXS-sized wound retractor. In addition, a 3-mm rigid port was inserted through the 5-mm incision. Moreover, we made a 1-cm skin incision to insert the thoracoscope into the fifth intercostal space along the anterior axillary line. Preoperative thoracic drainage was performed using the 1-cm skin incision. If not, we created a new thoracoscopic port in the same position. Our team initially conducted a single-arm study showing the feasibility and safety of the thoracoscopic transareolar approach in 10 consecutive patients. In all patients of the study, the postoperative drainage duration was 1 day, the postoperative hospitalization duration was 2 days, and there were no complications. Moreover, on postoperative day (POD) 7, the mean numerical rating scale score was 3.2; at postoperative month (POM) 12, all patients were pain-free. Subsequently, we prospectively compared the transareolar and uniportal approaches for thoracoscopic lung bullectomy (10). There were no significant differences between the transareolar and uniportal thoracoscopic approaches in terms of the perioperative outcomes, including operative time, intraoperative blood loss (minimal for all patients), duration of postoperative drainage (1 day for all patients), length postoperative hospital stay (2 days for all patients), complication rate (0% for all patients), or 1-year recurrence rate. Between the groups, the numerical rating scale pain scores on POD 7 and POM 12 were statistically similar. Finally, cosmetic satisfaction was evaluated using a 4-point scale (1, poor; 2, not good; 3, good; 4, excellent). Patients undergoing the transareolar approach had higher satisfaction scores than those who underwent the uniportal approach on POD 7 (t, 3.5±0.6 vs. u, 2.9±0.9; P=0.02) and POM 12 (t, 3.8±0.5 vs. u, 3.3±0.9; P=0.0065). Therefore, patients have greater cosmetic satisfaction after transareolar pulmonary bullectomy than the uniportal approach with equivalent perioperative outcomes and postoperative pain.
Several previous studies have described the use of the thoracoscopic transareolar approach for general thoracic surgery (11-14), including wedge resections for bullae and lung nodules, and sympathectomy for primary palmer hyperhidrosis. Table 1 summarizes the results of previous and current studies. In previous studies, the transareolar approach used one or two skin incisions, whereas we used three incisions. Two studies described the usefulness of the thoracoscopic transareolar approach for pneumothorax (11,12). Xu et al. retrospectively compared the perioperative results, postoperative pain, and cosmetic satisfaction after thoracoscopic pulmonary wedge resection using the transareolar and conventional biportal approaches (11). The patients receiving the transareolar approach had the reduction of postoperative pain and higher cosmetic satisfaction than the biportal approach with the statistically similar other perioperative outcomes. In a single-arm retrospective study, Lin et al. performed thoracoscopic transareolar bullectomy in 112 male patients, and demonstrated that this minimally invasive approach was feasible and safe (12). Additionally, the postoperative outcomes, including pain and cosmetic satisfaction, were excellent at the 6- and 12-month follow-ups. Two other studies described the use of thoracoscopic transareolar sympathectomy for the treatment of primary palmer hyperhidrosis and reported excellent perioperative outcomes, reduced postoperative pain, and satisfactory cosmetic results (13,14).
Table 1
| Author | Study period | Study design | Number of patients | Disease/surgical procedure | Results |
|---|---|---|---|---|---|
| Xu et al. | January 2012 to December 2014 | Retrospective, comparative (vs. conventional two-port) | 197 (transareolar: 65, conventional two-port: 132) | Spontaneous pneumothorax or lung nodule/pulmonary wedge resection | Postoperative pain, paresthesia, and cosmetic satisfaction were better after the transareolar approach |
| Lin et al. | January 2013 to December 2014 | Retrospective, single arm | 112 | Spontaneous pneumothorax/pulmonary wedge resection | Good perioperative outcomes, including postoperative pain and cosmetic satisfaction (no comparison) |
| Chen et al. | May 2012 to May 2014 | Single arm | 85 | Primary palmer hyperhidrosis/thoracic sympathectomy | Good perioperative outcomes, including postoperative pain and cosmetic satisfaction, and no recurrent symptoms of primary palmer hyperhidrosis (no comparison) |
| Lin et al. | January 2019 to September 2019 | Prospective, randomized, comparative (vs. single-port on axillary line) | 118 (transareolar: 58, single-port on axillary line: 60) | Primary palmer hyperhidrosis/thoracic sympathectomy | Postoperative pain and cosmetic satisfaction were better after the transareolar approach Other perioperative outcomes were equivalent between the two groups |
| Igai et al. | April 2018 to July 2019 | Prospective, open-label, comparative (vs. single-port on axillary line) | 40 (transareolar: 21, single-port: 19) | Spontaneous pneumothorax/pulmonary wedge resection | Postoperative pain and other perioperative outcomes were equivalent between the two groups Cosmetic satisfaction was better after the transareolar approach |
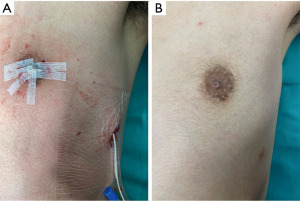
Most previous studies reported higher cosmetic satisfaction after the transareolar than comparative approach, which involved an incision on the lateral axillary line (10,11,13). Moreover, the areolar incision was not visible at POM 6. Compared to patients undergoing thoracic surgery for other diseases, those undergoing surgery for PSP are younger and place greater emphasis on cosmetic satisfaction. The cosmetic satisfaction of patients is a major advantage of the transareolar approach. Figure 1 demonstrates the postoperative courses of surgical wounds of a patient receiving the transareolar approach.
In female PSP patients, the transareolar approach is contraindicated, which makes it less applicable to the general population, whereas the conventional uniportal approach involving a single incision on the lateral axillary line can be used for both males and females. Therefore, the transareolar approach might not be useful for other diseases, such as primary and metastatic lung cancer, because of the lack of significant sex differences, although it may be a better option for standard treatment of young males with PSP.
In the transareolar approach, we penetrate mammary fat tissue, which may lead to mastitis. However, any local wound complications, such as mastitis, were not reported in previous studies (9-14). Therefore, we consider that mastitis is not a major concern when we perform the transareolar approach. Moreover, there are no reports describing other specific complications related with the transareolar approach.
Conclusions
In conclusion, the thoracoscopic transareolar approach is associated with higher cosmetic satisfaction, good postoperative pain relief, and equivalent perioperative outcomes compared to the conventional approach. Therefore, the transareolar approach might be preferred for the treatment of young males with PSP.
Acknowledgments
The authors thank the surgeons involved in the study, their coworkers, and the editors and reviewers for their assistance with the manuscript.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Kenji Tsuboshima) for the series “Single-Port VATS for Pneumothorax” published in Video-Assisted Thoracic Surgery. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://vats.amegroups.com/article/view/10.21037/vats-22-29/coif). The series “Single-Port VATS for Pneumothorax” was commissioned by the editorial office without any funding or sponsorship. HI serves as an unpaid Associate Editor-in-Chief of Video-Assisted Thoracic Surgery from December 2020 to November 2024. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sedrakyan A, van der Meulen J, Lewsey J, et al. Video assisted thoracic surgery for treatment of pneumothorax and lung resections: systematic review of randomised clinical trials. BMJ 2004;329:1008. [Crossref] [PubMed]
- Tsuboshima K, Wakahara T, Matoba Y, et al. Single-incision thoracoscopic surgery using a chest wall pulley for lung excision in patients with primary spontaneous pneumothorax. Surg Today 2015;45:595-9. [Crossref] [PubMed]
- Song IH, Lee SY, Lee SJ. Can single-incision thoracoscopic surgery using a wound protector be used as a first-line approach for the surgical treatment of primary spontaneous pneumothorax? A comparison with three-port video-assisted thoracoscopic surgery. Gen Thorac Cardiovasc Surg 2015;63:284-9. [Crossref] [PubMed]
- Ocakcioglu I, Alpay L, Demir M, et al. Is single port enough in minimally surgery for pneumothorax? Surg Endosc 2016;30:59-64. [Crossref] [PubMed]
- Qin SL, Huang JB, Yang YL, et al. Uniportal versus three-port video-assisted thoracoscopic surgery for spontaneous pneumothorax: a meta-analysis. J Thorac Dis 2015;7:2274-87. [PubMed]
- Nachira D, Ismail M, Meacci E, et al. Uniportal vs. triportal video-assisted thoracic surgery in the treatment of primary pneumothorax-a propensity matched bicentric study. J Thorac Dis 2018;10:S3712-9. [Crossref] [PubMed]
- Igai H, Kamiyoshihara M, Ibe T, et al. Single-incision thoracoscopic surgery for spontaneous pneumothorax using multi-degrees of freedom forceps. Ann Thorac Cardiovasc Surg 2014;20:974-9. [Crossref] [PubMed]
- Yoshikawa R, Matsuura N, Igai H, et al. Uniportal approach as an alternative to the three-portal approach to video-assisted thoracic surgery for primary spontaneous pneumothorax. J Thorac Dis 2021;13:927-34. [Crossref] [PubMed]
- Yazawa T, Igai H, Ohsawa F, et al. Feasibility of thoracoscopic pulmonary bullectomy using a transareolar approach for treatment of primary spontaneous pneumothorax. J Thorac Dis 2020;12:5794-801. [Crossref] [PubMed]
- Igai H, Kamiyoshihara M, Furusawa S, et al. A prospective comparative study of thoracoscopic transareolar and uniportal approaches for young male patients with primary spontaneous pneumothorax. Gen Thorac Cardiovasc Surg 2021;69:1414-20. [Crossref] [PubMed]
- Xu K, Bian W, Xie H, et al. Single-port video-assisted thoracoscopic wedge resection: novel approaches in different genders. Interact Cardiovasc Thorac Surg 2016;23:202-7. [Crossref] [PubMed]
- Lin JB, Chen JF, Lai FC, et al. Transareolar pulmonary bullectomy for primary spontaneous pneumothorax. J Thorac Cardiovasc Surg 2016;152:999-1005. [Crossref] [PubMed]
- Lin JB, Kang MQ, Chen JF, et al. Transareolar single-port endoscopic thoracic sympathectomy with a flexible endoscope for primary palmar hyperhidrosis: a prospective randomized controlled trial. Ann Transl Med 2020;8:1659. [Crossref] [PubMed]
- Chen JF, Lin JB, Tu YR, et al. Nonintubated transareolar single-port thoracic sympathicotomy with a needle scope in a series of 85 male patients. Surg Endosc 2016;30:3447-53. [Crossref] [PubMed]
Cite this article as: Igai H, Kamiyoshihara M. Thoracoscopic transareolar approach for primary spontaneous pneumothorax in young male patients. Video-assist Thorac Surg 2023;8:3.


