Uniportal video-assisted thoracoscopic pulmonary segmentectomy: a systematic review
Introduction
Lung cancer management has witnessed major changes in the last decade, especially in the form of minimally invasive approaches and robotic surgery. One such significant development is the uniportal video-assisted thoracoscopic surgery (VATS). Along with an increased interest in minimalistic approach, there has been a recent rise in the interest towards conservative approaches, especially for early stage lung cancers. The initial trial of lobectomy vs. sublobar resections (1) conducted more than decades before, now stands outdated and obsolete, given the advancement in radiological advancement in the form of better imaging facilities, which pick up more and more early lesions. Also the recent published set of data though retrospective in nature, on use of sublobar resections for early stage lung cancer, support the use of sublobar resections especially segmentectomy (in select cases) (2). Newer trials are at present evaluating the validity of sublobar resection in the present scenario (3).
Segmentectomy is a demanding procedure, requires a very good knowledge of anatomy, the vessels and its branches with bronchial divisions to help target the necessary portion of lung with minimal damage to the rest of the parenchyma. Segmentectomy by uniportal technique is further demanding, combining the advantages of both minimally invasive and conservative approach.
There have been only few centres in the world which routinely practice uniportal segmentectomy and only a few articles have been published in detail. Most of the publications have been case reports describing the technique of a particular segmentectomy. There is a lack of large volume published data on uniportal segmentectomy. In this review article we look into the literature available as on date, in the indexed journals, describing uniportal segmentectomy. We are not discussing the techniques of segmentectomy which are discussed in another publication from our centre (4).
Methods
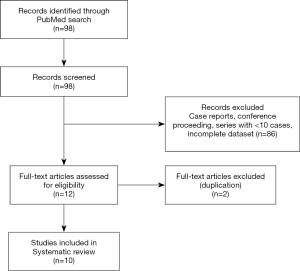
Electronic search was performed in PubMed for the terms “Uniportal segmentectomy”, “Single port Thoracoscopic Segmentectomy” on 12.8.2019. After initial review, relevant full text articles were retrieved. Eligible studies included all original articles and case series publications, which described the results of uniportal segmentectomy of lung. Case reports, editorial publications, conference proceedings in the form of abstracts, expert opinions were excluded from analysis. Case series describing <10 cases were excluded from the analysis. Studies describing combinations of segmentectomy with other resections (lobectomy/wedge), without separate data on uniportal segmentectomy were also excluded from the analysis (PRISMA diagram, Figure 1).
Data from the publications were retrieved, reviewed and analysed independently by the two authors (B Venkitaraman and L Jiang). Any disparities in the observations between the two observes were discussed and resolved and the final consensus is presented here. Statistical analysis was done using SPSS Statistics for windows version 17.0 (SPSS Inc. , Chicago, USA).
Results
A total of 98 articles were identified on initial search. After initial review, and removal of case reports and articles with incomplete dataset, 12 articles were found to satisfy the inclusion criteria for this review and were further analysed. Two were removed for possible repetition of cases. All the studies included were non randomised studies from single surgical centre, reporting their experience in the uniportal segmentectomy. Of the 10 studies three were comparative studies, comparing uniportal with multiport VATS segmentectomy while the rest evaluated only uniportal series (Table 1).

Full table
Indications
The most important part of surgical management is the selection of right cases. Various studies have described different selection criteria for patients undergoing uniportal VATS segmentectomy. The consistent features among these include:
- Benign or suspected benign lesion, where wedge is not feasible;
- Inflammatory lesions where segmentectomy can offer preservation of lung parenchyma;
- Metastatic lesions to lung not amenable to wedge resection;
- Ground glass lesions with solid component <50%, bilateral lesions;
- For patients with early stage lung cancer especially for tumour size <2 cm;
- Segmentectomy may be done in select patients who will not be fit for lobectomy due to their pulmonary compromise.
- Of late more and more patients with lesions <2 cm in peripherally placed lesions with no nodes have undergone segmentectomy especially if margin of 2 cm at least can be achieved after segmentectomy (4,5,7,13).
Routine contraindications include presence of dense adhesions, where visualisation of anatomy is difficult. The same also depends on the expertise of the surgeon and his team.
Presence of visceral pleural invasion is still an unclear entity and use of segmentectomy in these patients may be guardedly used. Presence of positive nodes has also been considered as an indication for completion lobectomy in patients with non-small cell lung cancer.
Learning curve
Minimally invasive procedures, need a longer time for reaching the plateau of learning curve. segmentectomy is a technically demanding procedure and performance by uniportal adds to the complexity. Among the published literature, few have analysed their outcomes over the years of experience and it was found that with performance of close to 33 procedures, surgeons reached the plateau of learning curve (5). Duan et al. also found that operative time, blood loss and localisation rates were significantly lower with increase in the experience in their study (13).
Techniques of identification of intersegmental plane
The important aspect of segmentectomy is the identification of the intersegmental plane, so that appropriate parenchymal division can be made. There have been different techniques described (7). The inflation deflation technique has been the most commonly applied technique (7) for identification of the intersegmental plane for parenchyma resection. After inflation and an application of stapler to divide a segmental bronchus and deflation, the target parenchyma remains inflated, helping us define the boundaries for resection. The downside of using this procedure is that vision gets obscured in the process of lung inflation and also presence of any collaterals can alter the inflation/deflation and lead to incorrect extent of parenchymal division.
Han et al. used intra operative bronchoscopy along with the above described technique to confirm the choosing of right bronchial division before performing the segmentectomy (7). Other techniques described in literature include open inflation technique (4), where in a bronchotomy of the segmental bronchus to be resected is done and the segment parenchyma alone is inflated using a deep vein catheter to inflate the segmental parenchyma and to define the plane. Others include use of 3D reconstruction of the segmental anatomy preoperatively as described by Xu et al. They utilised the system of 3D reconstruction of CT images prior to surgery using IQQA-3D analysis system. They compared the application of the 3D reconstruction system to non-application in uniportal VATS segmentectomy. They identified 57.3% segmental structure variations applying the software, most of these were single structure variations (69.1%) and most were segmental artery variations. On comparing the two groups, they found that even complicated surgeries could be performed without increase in the intraoperative time using preoperative 3D reconstruction. Thus, 3D technique was useful in the easy conduct of segmentectomy. They also used inflation deflation technique for identification of intersegmental plane (9).
Localisation of tumour
Yang et al. described technique of needlescopic localisation of the tumour preoperatively (8). These helped in exact localisation of non-palpable lesions and help in targeted excision. Hook wire placement was also performed in the series by Duan et al. (13). These were placed within two cm of the suspected lesion, under CT scan guidance. However, in the series from Shanghai pulmonary hospital, the placement of guidewire was only done, when it was difficult to exactly localise the lesion to a particular anatomical segment. This helps in guided resection and also in guided pathological assessment at Frozen section analysis (4).
Preoperative patient parameters
The mean age of patients included in the study ranged from 52 to 71.06 years. Most of these studies were performed on elective segmentectomy, on patients who were otherwise fit. This is based on the published preoperative pulmonary function tests results, where preoperative FEV1% was found to be more than 70% (4,8-10,12). Preoperative comorbid illness was also described in few studies and ranged from 31.1% to 52.5%. Contrary to the studies from West, the smoking prevalence was significantly low—ranging from 12.5% in most studies, going up to 24.2% (4,6,8,9,11,13). Most of these patients were also non-obese with BMI of patients being around 24 (4,6,8). The details of preoperative patient condition are described in detail in the Table 2.
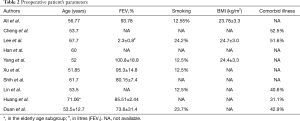
Full table
Operative parameters
All the surgeries were performed starting with uniportal VATS technique with a 4-cm incision on the chest wall and using special double-jointed instruments. The operative time ranged from 128 to 198 minutes in different series. Duan et al. in their analysis showed that the operative time and mean blood loss was significantly lesser in the latter part of the study (13). Cheng et al. analysed their patients in four temporal divisions and found similar outcomes, lowering of operative time and blood loss with increasing experience (5).
In the three studies which compared uniportal with conventional multiport segmentectomy, there was no significant difference between the two techniques with respect to the operative time (6,7,10). Lee et al. alone described a significant lower intraoperative blood loss with uniportal technique (6). Lee et al. described a conversion rate of 9% from uniportal to multiport technique, while Han et al. and Shih et al. described no multiport conversion. Conversion to open thoracotomy was in the range of 1.9–5.8% (6,7,10). Most common reason for conversion was dense adhesions obscuring the anatomy and intraoperative bleeding. There was no difference between the uniportal and multiport group in terms of conversion rates to thoracotomy (6). There were also few cases of conversion to lobectomy, because of inability to identify the lesion Intraoperatively (2.9–4.2%) (7,8). The comparative studies also revealed no significant difference in the number of nodes resected between the uniportal and conventional techniques of VATS segmentectomy (6,7,10). All these emphasise the fact that uniportal segmentectomy is as effective as multiport conventional VATS surgery.
The details of operative parameters observed in various studies are further in Table 3.
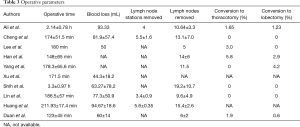
Full table
Postoperative outcome
Mean postoperative stay in the hospital among the various studies ranged from 4 to 7.4±1.9 days. The reported mean duration of intercostal drainage was between 2–5.9 days. In the comparative studies between uniportal and multiportal by Lee et al. and Han et al. , the uniportal arm had a significantly lesser duration of chest tube drainage and postoperative stay compared to multiport arm, an important post-operative parameter in favour of uniportal surgery. There was no reported 30-day mortality in any of the studies. The postoperative complication rates varied from as low as 4.2% to as high as 21.2% in the studies included. The most common postoperative complications reported in the studies included prolonged air leak (6,7), arrhythmias (4), postoperative lung infections (11,12) (Table 4).
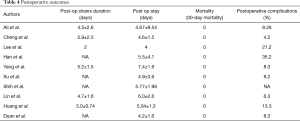
Full table
Histopathological analysis
The postoperative Histopathological analysis was well documented in many of the studies. The majority of these studies had reported having preinvasive tumours (Adenocarcinoma in situ) and T1 (mi) (minimally invasive adenocarcinoma (as per the AJCC 8.0 edition staging system) in the final operative specimen. The presence of adenocarcinoma in situ ranged from 4.5% to as high as 39.1% (9,13). Ali et al. also reported a high percentage of AIS (36.36%) (4). Minimally invasive adenocarcinoma defined as adenocarcinoma (≤3 cm in greatest dimension) with a predominant lepidic pattern and ≤5 mm invasion in the greatest dimension in the recent AJCC 8.0 Classification and is staged as T1 (mi). This was reported as high as 71.4% and 84.37% in the studies (9,11). Invasive adenocarcinoma was found comparatively lesser in number ranging from 9.38% to 31.82% (4,11). Many studies had reported the histopathology report in terms of stage of tumour. The majority of the studies had stage 1 tumours (4,6,10-12). Most of the tumours were small in size with the mean size of the tumour ranging from 0.7 to 2.15 cm, most of them being less than 2 cm in dimension (Table 5).
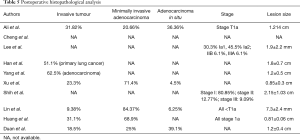
Full table
These pathological reports further justify the use of segmentectomy in these patients, as majority of them were early stage lung cancers. In many of the studies a formal mediastinal nodal dissection was included as a part of the surgery, after an intraoperative frozen or in patients with preoperative diagnosis of lung cancer.
Limitations
A major limitation in all of these studies is the lack of reporting of long-term survival, among patients undergoing segmentectomy (sublobar resection) for lung cancer. None of these studies have reported a methodical follow up plan and none of them reported the time of recurrence and site of recurrences. The availability of this survival analysis and recurrence pattern analysis will help further favouring or refuting the use of segmentectomy for early stage lung cancers and will also help in modifying the treatment regimes.
Conclusions
In this review, the articles included show a low and acceptable rate of post-operative morbidity with no 30-day mortality for uniportal segmentectomy, suggesting that uniportal segmentectomy for early stage lung cancer is feasible and safe in terms of post-operative outcomes, in experienced centres. Most of the studies also report an acceptable level of lymph node dissection in the mediastinum and hilum, thus proving uniportal approach to segmentectomy to be oncologically sound. Most of these studies have included patients who have small tumours, majority with lesion size <2 cm. Adenocarcinoma in situ and minimally invasive adenocarcinoma (reclassifications of bronchoalveolar type lung cancer), have been reported more commonly compared to invasive adenocarcinoma in many of the studies. These have been reported to have very good survival rates after complete surgical removal. These values suggest that uniportal segmentectomy may be performed on patients with tumors <2 cm and in those suspected to have lesser invasive variants. In future long-term analysis of Survival and recurrence will further confirm the long-term utility of uniportal segmentectomy in early stage lung cancer patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Kazuo Yoshida) for the series “Robotic VS Uniportal VATS” published in Video-Assisted Thoracic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats-19-57). The series “Robotic VS Uniportal VATS” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [Crossref] [PubMed]
- Altorki NK, Yip R, Hanaoka T, et al. Sublobar resection is equivalent to lobectomy for clinical stage 1A lung cancer in solid nodules. J Thorac Cardiovasc Surg 2014;147:754-62; Discussion 762-4. [Crossref] [PubMed]
- Altorki NK, Wang X, Wigle D, et al. Perioperative mortality and morbidity after sublobar versus lobar resection for early-stage non-small-cell lung cancer: post-hoc analysis of an international, randomised, phase 3 trial (CALGB/Alliance 140503). Lancet Respir Med 2018;6:915-24. [Crossref] [PubMed]
- Ali J, Haiyang F, Aresu G, et al. Uniportal Subxiphoid Video-Assisted Thoracoscopic Anatomical Segmentectomy: Technique and Results. Ann Thorac Surg 2018;106:1519-24. [Crossref] [PubMed]
- Cheng K, Zheng B, Zhang S, et al. Feasibility and learning curve of uniportal video-assisted thoracoscopic segmentectomy. J Thorac Dis 2016;8:S229-34. [PubMed]
- Lee J, Lee JY, Choi JS, et al. Comparison of Uniportal versus Multiportal Video-Assisted Thoracoscopic Surgery Pulmonary Segmentectomy. Korean J Thorac Cardiovasc Surg 2019;52:141-7. [Crossref] [PubMed]
- Han KN, Kim HK, Choi YH. Comparison of single port versus multiport thoracoscopic segmentectomy. J Thorac Dis 2016;8:S279-86. [PubMed]
- Yang SM, Wu WT, Liu YH, et al. Needlescopic-assisted uniportal video-assisted thoracoscopic pulmonary anatomical segmentectomy. J Vis Surg 2017;3:138. [Crossref] [PubMed]
- Xu G, Chen C, Zheng W, et al. Application of the IQQA-3D imaging interpretation and analysis system in uniportal video-assisted thoracoscopic anatomical segmentectomy: a series study. J Thorac Dis 2019;11:2058-66. [Crossref] [PubMed]
- Shih CS, Liu CC, Liu ZY, et al. Comparing the postoperative outcomes of video-assisted thoracoscopic surgery (VATS) segmentectomy using a multi-port technique versus a single-port technique for primary lung cancer. J Thorac Dis 2016;8:S287-94. [PubMed]
- Lin Y, Zheng W, Zhu Y, et al. Comparison of treatment outcomes between single-port video-assisted thoracoscopic anatomic segmentectomy and lobectomy for non-small cell lung cancer of early-stage: a retrospective observational study. J Thorac Dis 2016;8:1290-6. [Crossref] [PubMed]
- Huang L, Zheng B, Chen C, et al. To Explore Clinical Value of Single-port Video-assisted Thoracoscopic Surgery in Elderly Patients With Non-small Cell Lung Cancer: Lobectomy, Segmentectomy and Lobectomy vs Segmentectomy. Zhongguo Fei Ai Za Zhi 2018;21:287-95. [PubMed]
- Duan L, Jiang G, Yang Y. One hundred and fifty-six cases of anatomical pulmonary segmentectomy by uniportal video-assisted thoracic surgery: a 2-year learning experience. Eur J Cardiothorac Surg 2018;54:677-82. [Crossref] [PubMed]
Cite this article as: Venkitaraman B, Cai J, Ma X, Chen Z, Shi Z, Jiang L. Uniportal video-assisted thoracoscopic pulmonary segmentectomy: a systematic review. Video-assist Thorac Surg 2021;6:4.