Feasibility, safety and effectiveness of videothoracoscopy with local anesthesia and sedation without tracheal intubation
Introduction
Thoracoscopy (TP) is an effectively method in diagnostics and therapies in the pleural cavity, which has shown a 95% effectiveness rating in all its indications (1). Before the advent of anti-tuberculosis drugs, the performance of TP was already discussed to promote pneumothorax in patients who suffered from tuberculosis and in adhesiolysis, for the purpose of promoting pulmonary expansion in patients who suffered from this disease (2).
Introducing the videothoracoscopy (VT) and its increased utilization, which had a significant impact on the process of thoracic surgery in the last 30 years, as it benefited thousands of patients with a lesser degree of morbidity, lower incidence of post-operative pain, shorter length of stay at the hospital and earlier return to activities (3-5). The advent of safe anesthesia, cameras with optic fibers, and articulated staplers made it possible to perform larger procedures using video-assisted thoracic surgery. General anesthesia was incorporated into modern techniques (6). The evolution of VT up to its current status, makes it possible for the thoracic surgery to treat various diseases injuring the thorax and employing minimally invasive techniques (7).
Nowadays, VT is a widely used procedure in thoracic surgery and general anesthesia is a standard practice for this purpose, including selective tracheal intubation (double lumen pulmonary ventilation tube), whereas it is generally necessary to block the lung on the side being operated (6,8). We have based the principle on the concept that some procedures do not necessarily require general anesthesia, thereby avoiding some risks from the anesthetic method, as well as those derived from simple tracheal intubation and, especially from the selective one (6,8). The idea of thoracoscopy combined with local anesthesia has been employed since the beginning of the procedure with Jacobeus. Rusch and Mountain revived it in 1987, because of the report on the performance of thoracoscopy on pleura diseases without general anesthesia. Whereas several intercostal blockers and a standard mediastinoscopy were utilized, inserted through the intercostal space, performing the diagnosis and treatment of pleural diseases on 46 patients (9). One decade after that, Nezu et al. published a series on 34 consecutive patients submitted to marginal resection of the subpleural bullae for the treatment of spontaneous pneumothorax. All of these cases were performed by thoracoscopy under local anesthesia and sedation (10). Migliore et al. in 2002 tried a “formula for the procedure”, but they still tried to perform it without sedation. However, no comment was made on the clinical behavior of the operated population during the VT in the cases studied (11).
The present study evaluates the feasibility, safety and effectiveness of VT under local anesthesia and sedation, and if the proposed procedure in the study is acceptable for this purpose: the diagnostics or treatment of the disease which prompted the indication for VT. Furthermore to know if VT combined with local anesthesia and sedation can be considered as a feasible option for this purpose.
Methods
Sixty eight patients were operated between 2009 and 2016, which were indicated for a possibility of the thoracic procedure performed by VT, whether it is for diagnostic or treatment purposes of a pleural, pulmonary, or mediastinal disease. All the patients who were included in the study group had given their consent and signed the statement of informed consent [the study was approved by the Research Ethics Committee at the Federal University of São Paulo (study 1588/08)]. The surgeries were performed consecutively by the same surgeon but with different anesthetic teams. All the anesthesiologists followed the established sedation protocol for the project.
When the patients arrived at the surgical center, 0.02 mg/kg of midazolam (pre-sedation) and 2 g of cefazolin (for the infection prophylaxis) were administered intravenously. After a 10 minutes infusion of the pre-sedation, the patients were transferred to the operating room and, on the operating table; the pulse oximetry, electrocardioscopy, and noninvasive BP were monitored again. At this time, continuous oxygen was administered using a simple facial mask at 3 L/min. Then, the patient was properly monitored, the initial values were collected from the following parameters: O2 Sat by pulse oximetry; BP; HR; sedation level measured by the subjective RSS (12). After the vital sign parameters were collected and registered, fentanyl was administered intravenously, a dosage of 1.5 mcg/kg. This moment was standardized in this study as “time 0” (the time the infusion of fentanyl began), when the stopwatch started to measure the elapsed time of the surgery.
After the antisepsis was concluded, the surgical field was prepared, and the checking of the VT was done, then the continuous infusion of propofol was started at a dosage of 0.05 mg/kg/min. Beginning at this time, the parameters were measured every three minutes: O2 Sat, BP and HR until the procedure was concluded. The sedation level, based on the subjective RSS, was measured every nine minutes until the procedure was concluded (removal of the last trocar). The data from the trocars at the time of insertion and the respective variations of the vital signs at the exact time of the surgery was also collected.
The access to the pleural cavity by VT was also performed on the patient when positioned on lateral decubitus. The insertion point of the optical trocar was anesthetized using a 1% lidocaine solution, in the sixth or seventh intercostal space, varying the infused solution volume from 8 to 15 mL, depending on the thickness of the thoracic wall of each patient, anesthetizing from the skin to the parietal pleura. Either a 5.5 or a 10.5 mm trocar (depending on the diameter of the selected optical instrument) was positioned in the anesthetized site, after air had been injected into the pleural cavity (approximately 60 mL—in patients without pleural effusion), in such way to allow the safe insertion of the 5 or 10 mm VT optical instrument at 30 degrees inside the pleural cavity.
The diagnostic or therapeutic procedures in the pleural cavity or the surfaces of the lung was started by positioning the optic instrument in the pleural cavity, allowing to choose the best and required location for inserting the second or third trocar to perform the procedure. Applying the same technique of local anesthesia using 1% lidocaine to insert each extra trocar which is necessary for aspiration, inserting the surgical tweezers or staplers.
After each operation, data was collected on the following parameters evaluating the effectiveness and feasibility of the method: whether there was any kind of memory of pain or discomfort during the course of the operation; need for admittance to the ICU; diagnostics and treatment: if the procedure supplied the anatomopathological diagnosis necessary for the performance of the VT or, if it achieved the previously proposed necessary treatment. The safety of the procedure was evaluated by the necessity for tracheal intubation during the course of the surgical act, variations in the vital signs that could put the patient in danger or the occurrence of death directly related to the procedure.
The following variables were analyzed: O2 Sat, BP, HR (checked every three minutes), RSS (evaluated every nine minutes), the insertion of the trocars and if this is related to the vital signs variations. The statistical analysis was performed based on the vital sign variations during the course of the procedure, among all the patients in the study, comparing the O2 Sat, BP (diastolic and systolic), and HR in each time. The data was collected on the “time line” beginning at the time “0” starting point, considering this moment as the beginning of the surgical process. Statistical analysis was also performed at the time the trocars were introduced and the changes caused in the vital signs at the time “0” starting point. The analysis of the total sample was analyzed, as well as the patients were divided into groups for comparative study: male and female; patients 60 years old or younger (≤60 years) and older than 60 years (>60 years); patients with and without cardiovascular risk; patients with previous malign neoplasm, with functional capacity level ≤2 and > 2 on the ECOG scale (12).
A P value less than 0.05 was considered statistically significant. Statistical analysis was performed using SPSS—Statistical Package for Social Sciences—IBM SPSS Statistics 18.
Results
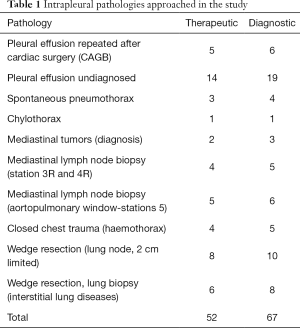
The procedure was performed successfully on 67 operated patients, and the prospectively collected clinical data was collected: (42 women and 26 men); the average age was 54.48±20.41 [19–79]. The average surgical time was 21.91 minutes. It was not necessary to perform tracheal intubation, convert to open surgery or admission to the ICU. The average hospital stay was 2.2 days (16 hours to 4 days), the patients were released from the hospital after the chest tube was removed. All the patients reported having no memory of the surgical act, neither any memory of related pain nor discomfort. Diagnostics was obtained in all cases when the need arose for diagnosis of the pleural disease. In patients whom were treated by VT for any disease, all of them achieved the expected results. In the intraoperative period were performed, besides the videothoracoscopic diagnosis, intracavitary procedures indicated for each case: parietal pleural or visceral biopsies; pleurodesis with talc insufflation; pulmonary biopsies; marginal resection of subpleural apical “blebs”; mediastinal tumor; aspiration of the intrapleural coagulations (hemothorax – trauma). There were no deaths related to the procedure, intraoperative or up to 30 days after the surgery (Table 1).
Full table
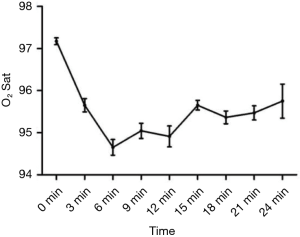
The sample displayed a drop in the O2 Sat in the first six minutes of the procedure, but then there was a significant recuperation in the values as it approached the end. The O2 Sat remained stable right before the insertion of the trocars, without any significant change. There was no significant variation in the O2 Sat during the entire time of the procedure (Figure 1).
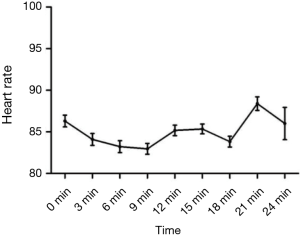
Who were over 60 years old and the group that displayed a certain degree of cardiovascular risk presented a significant change in the O2 Sat (P<0.05), but without impact in clinical practice, as the patients remained with satisfactory levels of O2 throughout the entire course of the surgery, considering it was not necessary to perform tracheal intubation at all. The O2 Sat remained stable before and after the insertion of the trocars, without any significant change. The variations in the BP systolic and diastolic initially dropped statistically significant, but there was no decrease in tissue perfusion: hemodynamic support using vasoactive drugs or intravenous volume was not needed in any patient (Figure 2).
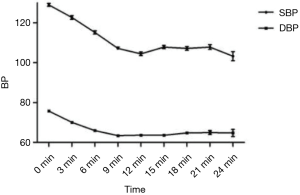
Only the group with previous oncological disease and with the worst functional capacity (ECOG >2), displayed a significant difference of this variable as related to the group with the better functional capacity (ECOG ≤2), for the systolic BP as well as the diastolic BP.
The observed factors that could change the HR, such as painful stimulus, did not display any significant results, even when there was a slight drop of HR after the sedation was begun. During the procedure, the successive stimuli, such as the insertion of the trocars and placement of the chest tube, did not display any significant effects. When we approached to the end of the procedure, there was a discrete rise of the HR, especially when the surgery exceeded 20 minutes, yet this did not cause any statistically relevant change or modified the evolution of the operated patients (Figure 3).
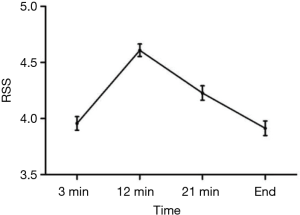
During the insertion of the trocars through the chest wall, no significant changes were observed in the vital signs or the appearance of a reflexive cough. No significant differences were found when comparing the O2 Sat and the HR at the time that preceded the insertion of the first trocar or immediately after the respective insertion, which was also verified when the second trocar was inserted. We consider that a good local anesthesia of the intercostal space and keeping the RSS between 3–5, were factors that contributed to the success at the time of greatest pain stimulus, occurred on the thoracic wall punction (Figure 4).
After the VT was performed under local anesthesia and sedation, the cancer patients in the study were capable of beginning chemotherapy or radiotherapy earlier, due to the same size of the incisions, when compared to the more invasive thoracic procedures performed under general anesthesia. Similar to Jiang et al. and Swanson et al., these patients were released earlier to begin chemotherapy less than 14 days post-operatively (13,14).
Discussion
The diagnostic achieved through VT is the greatest benefit when compared to closed pleural biopsies (by needle) and the cytology of pleural effusions, between 90 and 100%, when compared to cases that were not diagnosed. As De Camp et al., we were able to diagnose 100% of the cases performed in our study, by VT under local anesthesia and sedation (1). In cases where the patient was debilitated, the surgeon might find it difficult to indicate a more invasive procedure such as VT, nevertheless this method is always associated with general anesthesia, commonly performed by using selective tracheal intubation (9,15). This form of anesthesia can provoke general complications (cardiac arrhythmias, for example) and specific as laryngeal trauma, tracheal or bronchial lesion (16-18).
The attempt to perform VT using other modalities of anesthesia was encouraged in some procedures in thoracic surgeries (19-21). Rusch and Mountain already demonstrated this in 1987 by showing the benefits of performing thoracoscopy under local anesthesia for the diagnosis and treatment of pleural effusions, whereas a conventional mediastinoscopy was used to perform the procedure, which provided a greater diameter than the conventional VT camera and made it possible to get a direct view of the pleural cavity (9). This study was performed originating from the observation of debilitated patients, so that another option could be offered to those who were insecure about being submitted to general anesthesia and selective tracheal intubation, being aware of the seriousness of their condition, or just personal fear of being submitted to general anesthesia. Thus, it was possible to display a safer option of a combination of VT under sedation and local anesthesia, during the time in which the patient is submitted to the procedure. We could have an option for the patient who not accepts the idea of undergoing general anesthesia. Differently from Migliore et al., we have decided for to use local anesthesia on the thoracic wall only once, while this author dissected the wall by planes and would anesthetize it in steps: initially the skin followed by the subcutaneous cellular tissue, musculature and parietal pleura (11).
As the behavior of the patient’s vital signs were not expressed in publications during the time they were submitted to a VT under local anesthesia (with or without sedation). There was an interest in evaluating the vital signs of the patient during the performance of a VT under local anesthesia and sedation, and especially, at certain specific moments in this procedure when suddenly painful stimulus occurred (as when the trocars were inserted), seeking the significant variations of vital signs on the “time line” and, when possible, relating this variation to the patient’s pre-existing conditions (such as previous cardiac diseases, ECOG greater than 1, and over 60 years old). After the required evaluation of the “time line”, being then defined as the procedure safety, we have observed its respective effectiveness, if the results were similar to what was obtained in the VT procedure under general anesthesia. It is possible to observe from the studies by Landreneau et al., Mckenna et al. and Kaiser et al., who reported on the effectiveness and the safety of VT performed under general anesthesia for all indications of the procedure, low morbidity was observed due to the safety of this surgical method, as we found in our study performed under local anesthesia and sedation (7,22-25).
The majority of the research works found in the literature focuses only on the indication of VT under local anesthesia and sedation in some specific diseases, whereas very little information was observed on the vital signs during the surgical act in this anesthetic modality. Tschopp et al. and Alrawi et al., in 1997 and 2000 respectively, studied VT in the treatment of spontaneous pneumothorax and the diagnosis of pleural effusion, but how the patient evolved clinically during the surgery was not reported in these studies and, if there was any memory of pain during the course of the operation, but just the evaluation of the possible or not to perform the procedure. The inherent risks and benefits were only slightly or not even evaluated at all (26,27).
Yokoyama et al. studied the performance of VT under local anesthesia for diagnosing types of pleural infusion, in patients who suffered from pleurisies. In this research work, the only variable that was verified was the patient being asked if they suffered from pain or shortness of breath, while the patient in the study was completely conscious (28). In our study, besides performing the evaluations on vital signs during the procedure, we were careful to offer the patient comfort, providing the necessary previous sedation before putting the patient under local anesthesia in order to insert the trocars. Regarding a recent study, Katlic et al. reported in 2010 the performance of VT under local anesthesia and sedation in 384 cases, displaying satisfactory final results through this combination. Even in a representative number of cases, there is not commentary on the behavior of vital signs during the surgical act so, the doubt remains on how these patients evolved from the period when they entered the operating room until the conclusion of the procedure, or if they were satisfied with the method (29). In our study, we agree with Rusch et al. and Oak et al., where patients who have voluminous pleural infusions had already suffered from pulmonary collapse, thereby facilitating the insertion of the trocars (5,9).
The option for selecting the Ramsay Scale Score (RSS) was due to its practicality and objectivity as, it is widely known and used by anesthesiologists, which facilitates the collection of information from this professional who, besides performing his function of sedating the patient, had to collect all the data during the course of the procedure (30-33). The analysis every nine minutes made it possible the necessary circulation and metabolizing of the drugs used for sedation, and the necessary collection of data on the vital signs along the “time line” (31-34). Related to time “0”, we observed that the patients achieved satisfactory levels of sedation near the midpoint time of the procedure (12 minutes). Nearing the end of the operation, they regained the level of consciousness, with RSS values nearly equal to time “0”. As no patient needed advanced ventilatory support, we felt secure, even at Ramsay levels equal or greater than four.
One concern, in the study, was to analyze if the patient had any memory of pain or discomfort from the procedure. We focused on maintaining a sufficient level of sedation and amnesia while administering the smallest quantity of drugs as possible, in order to diminish the risk of the necessity of employing advanced ventilatory support, whenever needed. All the patients who were questioned the next day after the procedure denied any type of memory of the surgical act. Safety was well represented, as there was very little variation in the vital signs during the surgical act, as well as no patient needed any urgent tracheal intubation during the surgical act. Additionally to these facts, there was no need for any patient to be admitted to the ICU and also no deaths occurred related to the procedure or even 30 days subsequently.
Conclusions
VT under local anesthesia and sedation is feasible, safe and efficient. It was performed successfully and achieved its objective in the 23 patients who were studied, can be used for different kinds procedures in the pleural cavity. The surgery is safe, there was no need for tracheal intubation, admittance to the ICU and no death occurred to any patient in the study. The VT under local anesthesia and sedation is a feasible procedure, especially when the safety and comfort of the patient is analyzed in the operative and post-operative period, it can be a preferred option among the selected patients.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2019.07.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Research Ethics Committee at the Federal University of Sao Paulo (study 1588/08). All the patients who were included in the study group had given their consent and signed the statement of informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- De Camp PT, Moseley PW, Scott ML, et al. Diagnostic thoracoscopy. Ann Thorac Surg 1973;16:79-84. [Crossref] [PubMed]
- Bloomberg AE. Thoracoscopy in perspective. Surg Gynecol Obstet 1978;147:433-43. [PubMed]
- Detterbeck F. Thoracoscopic versus open lobectomy debate: the pro argument. Thorac Surg Sci 2009;6:Doc04. [PubMed]
- Santambrogio L, Nosotti M, Bellaviti N, et al. Videothoracoscopy versus thoracotomy for the diagnosis of the indeterminate solitary pulmonary nodule. Ann Thorac Surg 1995;59:868-70; discussion 870-71. [Crossref] [PubMed]
- Oak SN, Parelkar SV, Satishkumar KV, et al. Review of video-assisted thoracoscopy in children. J Minim Access Surg 2009;5:57-62. [Crossref] [PubMed]
- Ginsberg RJ. Preoperative assessment of the thoracic surgical patient: a surgeon’s viewpoint. In: Pearson FG, Deslauriers J, Ginsberg RJ, et al., eds. Thoracic Surgery. London: Churchill Livingstone, 1995:29-36.
- Kaiser LR, Shrager JB. Video-assisted thoracic surgery: the current state of the art. AJR Am J Roentgenol 1995;165:1111-7. [Crossref] [PubMed]
- Williamson JA, Webb RK, Szekely S, et al. The Australian Incident Monitoring Study. Difficult intubation: an analysis of 2000 incident reports. Anaesth Intensive Care 1993;21:602-7. [Crossref] [PubMed]
- Rusch VW, Mountain C. Thoracoscopy under regional anesthesia for the diagnosis and management of pleural disease. Am J Surg 1987;154:274-8. [Crossref] [PubMed]
- Nezu K, Kushibe K, Tojo T, et al. Thoracoscopic wedge resection of blebs under local anesthesia with sedation for treatment of a spontaneous pneumothorax. Chest 1997;111:230-5. [Crossref] [PubMed]
- Migliore M, Giuliano R, Aziz T, et al. Four-step local anesthesia and sedation for thoracoscopic diagnosis and management of pleural diseases. Chest 2002;121:2032-5. [Crossref] [PubMed]
- ECOG Performance Status [Eastern Cooperative Oncology Group web site]. July 27, 2006. Available online: http://ecog.dfci.harvard.edu/general/perf_stat.html, accessed January 16, 2012.
- Swanson SJ, Meyers BF, Gunnarsson CL, et al. Video-assisted thoracoscopic lobectomy is less costly and morbid than open lobectomy: a retrospective multiinstitutional database analysis. Ann Thorac Surg 2012;93:1027-32. [Crossref] [PubMed]
- Jiang G, Yang F, Li X, et al. Video-assisted thoracoscopic surgery is more favorable than thoracotomy for administration of adjuvant chemotherapy after lobectomy for non-small cell lung cancer. World J Surg Oncol 2011;9:170. [Crossref] [PubMed]
- Gilbert TB, Goodsell CW, Krasna MJ. Bronchial rupture by a double-lumen endobronchial tube during staging thoracoscopy. Anesth Analg 1999;88:1252-3. [Crossref] [PubMed]
- Riphaus A, Wehrmann T, Weber B, et al. S3-guidelines: sedation in gastrointestinal endoscopy. Z Gastroenterol 2008;46:1298-330. [Crossref] [PubMed]
- Paspatis GA, Manolaraki MM, Vardas E, et al. Deep sedation for endoscopic retrograde cholangiopancreatography: intravenous propofol alone versus intravenous propofol with oral midazolam premedication. Endoscopy 2008;40:308-13. [Crossref] [PubMed]
- Divatia JV, Bhowmick K. Complications of endotracheal intubation and other airway management procedures. Indian J Anaesth 2005;49:308-18.
- Martindale SJ. Anaesthetic considerations during endoscopic retrograde cholangiopancreatography. Anaesth Intensive Care 2006;34:475-80. [Crossref] [PubMed]
- Green SM, Krauss B. Procedural sedation terminology: moving beyond "conscious sedation". Ann Emerg Med 2002;39:433-5. [Crossref] [PubMed]
- Nelson D. Procedural sedation in the emergency department. In: Krauss B, Brustowicz RM. editors. Pediatric and Procedural Sedation and Analgesia. Baltimore: Lippincott Williams and Wilkins, 1999:161.
- Landreneau RJ, Mack MJ, Hazelrigg SR, et al. Video-assisted thoracic surgery: basic technical concepts and intercostal approach strategies. Ann Thorac Surg 1992;54:800-7. [Crossref] [PubMed]
- Kaiser LR. Video-assisted thoracic surgery. Current state of the art. Ann Surg 1994;220:720-34. [Crossref] [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Landreneau RJ, Hazelrigg SR, Mack MJ, et al. Postoperative pain-related morbidity: video-assisted thoracic surgery versus thoracotomy. Ann Thorac Surg 1993;56:1285-9. [Crossref] [PubMed]
- Tschopp JM, Brutsche M, Frey JG. Treatment of complicated spontaneous pneumothorax by simple talc pleurodesis under thoracoscopy and local anaesthesia. Thorax 1997;52:329-32. [Crossref] [PubMed]
- Alrawi SJ, Raju R, Acinapura AJ, et al. Primary thoracoscopic evaluation of pleural effusion with local anesthesia: an alternative approach. JSLS 2002;6:143-7. [PubMed]
- Yokoyama T, Toda R, Tomioka R, et al. Medical Thoracoscopy Performed Using a Flexible Bronchoscope Inserted through a Chest Tube under Local Anesthesia. Diagn Ther Endosc 2009;2009:394817 [Crossref] [PubMed]
- Katlic MR, Facktor MA. Video-assisted thoracic surgery utilizing local anesthesia and sedation: 384 consecutive cases. Ann Thorac Surg 2010;90:240-5. [Crossref] [PubMed]
- Henderson F, Absalom AR, Kenny GN. Patient-maintained propofol sedation: a follow up safety study using a modified system in volunteers. Anaesthesia 2002;57:387-90. [Crossref] [PubMed]
- Chainaki IG, Manolaraki MM, Paspatis GA. Deep sedation for endoscopic retrograde cholangiopacreatography. World J Gastrointest Endosc 2011;3:34-9. [Crossref] [PubMed]
- Ramsay MA, Savege TM, Simpson BR, et al. Controlled sedation with alphaxalone-alphadolone. Br Med J 1974;2:656-9. [Crossref] [PubMed]
- De Jonghe B, Cook D, Appere-De-Vecchi C, et al. Using and understanding sedation scoring systems: a systematic review. Intensive Care Med 2000;26:275-85. [Crossref] [PubMed]
- Oei-Lim VL, Kalkman CJ, Makkes PC, et al. Computer controlled infusion of propofol for conscious sedation in dental treatment. Br Dent J 1997;183:204-8. [Crossref] [PubMed]
Cite this article as: de Oliveira A, Perfeito JAJ, Girão MJBC, Shyu M. Feasibility, safety and effectiveness of videothoracoscopy with local anesthesia and sedation without tracheal intubation. Video-assist Thorac Surg 2019;4:17.