
Safe vascular and bronchial division techniques for VATS uniportal lung resections
Introduction
VATS anatomic resections for early stage non small cell lung cancers are becoming the standard of care with a record of at least equivalent safety, feasibility, oncological quality compared with open technique (1). Following the minimally invasive trend, uniportal VATS resections have been described in large case series (2) and results have been comparable to multi-portal VATS. Safe vascular division techniques using endoscopic roticulating staplers in triportal VATS have been described in detail (3), but uniportal VATS approach has unique challenges concerning a limited incision, vascular anatomy, angle of traction, stapler insertion and safe division. In this article, we are presenting a systemic description of technique for safe vascular and bronchial division for VATS uniportal anatomic resections.
All patients included in the article gave written consent for the use of anonymised medical data for scientific studies and also informed consent about the procedure per institutional protocol.
Surgical technique
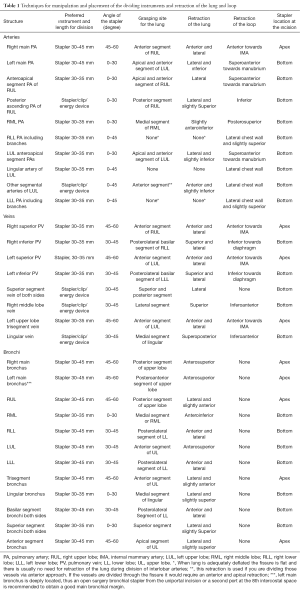
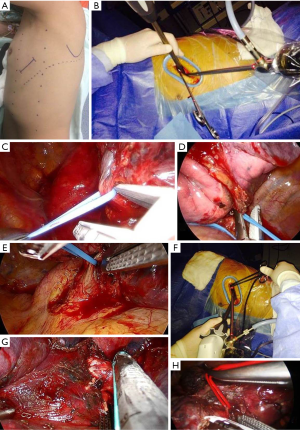
Forty six consecutive uniportal anatomic lung resections [left upper (n=6) and lower lobectomy (n=11), left upper trisegmentectomy (n=4), left pneumonectomy (n=1), right upper (n=11), middle (n=2) and lower (n=10) lobectomy] were performed by a single surgeon (HFB) since April 2014 using the described technique in Marmara University Hospital, Istanbul/Turkey. All patients underwent standard of care preoperative workup and clinical staging. After confirmation of single lung ventilation patients were placed in classic lateral decubitus position with an axillary roll in place. A 5-cm incision was performed between anterior and posterior axillary line at the 5th intercostal space (ICS). Ten or 5-mm 30 degree scopes, surgical instruments and endoscopic harmonic scalpel were used. After preparation of a vessel for division, a vascular tape was placed around the vessel and appropriate retraction was performed through manipulation of the vascular tape with a long curved clamp inside the thoracic cavity. This maneuver allowed easy and safe passage of the stapler behind the vessel. Retraction and manipulations for various vascular and bronchial structures are listed in Table 1. Figure 1 shows appropriate utility port placement (A), outside view and angulation of stapler, thoracoscope and lung retractor during division of pulmonary vein (B) and also various intrathoracic manipulations of structures prepared for division.
Full table
There were no instances of intraoperative vascular or bronchial injury or reoperation due to bleeding. In a left pneumonectomy case, a second port was opened at the 8th ICS posterior axillary line to achieve a short pneumonectomy stump. Lobectomy and pneumonectomy specimens were slid through the utility incision after being placed in a appropriately cut sterile serum bag. We did not encounter the need to enlarge the incision for the specimen but the ones with bigger (3–5 cm) tumors were considerably more difficult to pull out.
Discussion
Safe vascular division is the most critical point for VATS lobectomy/segmentectomy operations. Uniportal VATS approach imposes additional geometric challenges for stapler orientation and placement due to further restriction of access, equipment crowding and hilar anatomy. For classical VATS catastrophic intraoperative complications are reported at 1% (4). For uniportal operations the surgeon should be able to fit the operation according to the specific anatomy, as the uniport restricts otherwise appropriate classical actions.
Safe division during uniportal VATS resection depends on a few principles. There should be minimal instrument crowding and instruments should not apply pressure on each other. Such problems transfer the pressure and tension to anatomic structures and also cause pain through impingement of the intercostal nerve. Moreover, since most of the vascular preparation and exposure is done from the anterior side with the lung retracted posteriorly, traction of the vessel for division should be roughly opposite to the lung retraction to avoid harming of the posterior structures. This can not be achieved with a vascular tape manipulated outside the thorax, which causes an upwards retraction and an unfavorable angle for easy passage of a stapler. Classical bronchial closure technique involves meticulous alignment of membranous side to cartilaginous part (5) and also requires precise manipulation in minimally invasive setting (Table 1).
The described technique transfer the tension to a wider area on the vessel tape and prevents traction by the legs of the stapler. The tension is also distributed to lung surface with correct grasping and retraction of the lung. It enables us to safely pass the stapler even in instances of inability to gain vascular and bronchial length due to larger and more central tumors.
In conclusion, uniportal resections opens a new era when surgeons have to think of the geometry and tension distribution on the anatomic structures more than ever before. The technique described in this article follows these principles and is safe and effective.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Hasan Batirel, MD, PhD serves as a consultant for Johnson and Johnson and Marmara University Faculty of Medicine Department of Thoracic Surgery has an educational agreement with Johnson and Johnson.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). All patients included in the article gave written consent for the use of anonymised medical data for scientific studies and also informed consent about the procedure per institutional protocol.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nwogu CE, D'Cunha J, Pang H, et al. VATS lobectomy has better perioperative outcomes than open lobectomy: CALGB 31001, an ancillary analysis of CALGB 140202 (Alliance). Ann Thorac Surg 2015;99:399-405. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Park IK. Lobe-specific unidirectional stapling strategy in video-assisted thoracic surgery lobectomy. Surg Laparosc Endosc Percutan Tech 2012;22:370-3. [Crossref] [PubMed]
- McKenna RJ Jr. Complications and learning curves for video-assisted thoracic surgery lobectomy. Thorac Surg Clin 2008;18:275-80. [Crossref] [PubMed]
- Wright CD, Wain JC, Mathisen DJ, et al. Postpneumonectomy bronchopleural fistula after sutured bronchial closure: incidence, risk factors, and management. J Thorac Cardiovasc Surg 1996;112:1367-71. [Crossref] [PubMed]
Cite this article as: Bilgi Z, Batirel HF. Safe vascular and bronchial division techniques for VATS uniportal lung resections. Video-assist Thorac Surg 2017;2:4.


