
Uniportal S10 segmentectomy by transfissural intersegmental tunneling
Introduction
Isolated resection of the posterior basal segment (S10) is infrequent and considered of the most challenging anatomical segmentectomy when done by uniportal approach. First, the basal pulmonary artery branches are deeply located in the lung parenchyma making the identification of the segmental artery difficult, and division of two intersegmental planes is required. Furthermore, anatomical variations are very common in this region. Incorrect identification of vascular or bronchial structures and of the intersegmental plane may lead to potentially catastrophic complications or insufficient margins. The intersegmental tunneling method allows the early division of the intersegmental plane between S6 and S10 and the subsequent accurate identification of the segmental artery S10 and the dominant vein to S10. In this article, we describe the uniportal procedure for the right S10 segmentectomy by intersegmental tunneling.
Patient selection and work up
Posterior basal segmentectomy (S10) can be indicated in case of central metastases or non-solid tumors with ground glass opacity suggesting non-invasive lung cancer (1). However, saving lung parenchyma by a less invasive resection is related to a technically challenging procedure. Therefore, articles focused on thoracoscopic posterior basal segmentectomy are scarce (2-7). Perfect knowledge of anatomy is crucial for planning such complex segmentectomy and a thin slice Chest CT-scan with contrast product should be performed to identify anatomical variation. The trans-fissure technique requires an extensive dissection through the fissure to first individualize the lower lobe segmental arteries and then transect the bronchus and the veins. This technique could be indicated in NSCLC patients where extensive removal of all lymph nodes 12 and 13 can be realized. When the fissure is incomplete, the operation may be difficult and increase the risk of post-operative air leak.
Peri-operative setting
The general anesthesia is managed with a left double-lumen tube. The patient is positioned on lateral side and the table is flexed to increase the distance between the ribs. A 3-cm incision is performed in the 5th intercostal space between the tip of the scapula and the breast in the anterior axillary line. The wound is protected by a plastic soft tissue retractor (Alexis® Retractor Applied Medical USA).
The surgeon and the assistant are positioned on the anterior side of the patient whereas the scrub nurse stands at the back. A 10-mm 30º thoracoscope is used in order to optimize the visualization of the pleural cavity and all mediastinal structures. A dissector (Scanlan®, USA), a hook monopolar cautery and an Ultracision Harmonic scalpel (Ethicon®, Johnson & Johnson, USA) are used for dissection and coagulation respectively. All vessels are divided by endoscopic staplers (Golden Stapler®, DACH Medical Group, Germany). As mediastinal lymph node dissection is generic to all oncologic pulmonary resections, it is not described in this tutorial.
Procedure
Dissection starts in the middle portion of the major fissure where the artery is approached (Video 1). The basilar arterial trunk is exposed. All branches must be carefully dissected on a sufficient length to avoid misidentification. At this point, interlobar lymph nodes are totally removed.
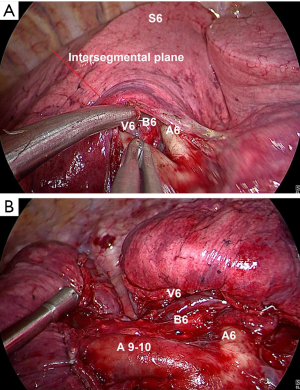
The common trunk for A9+10 and A6 (posteriorly) are clearly identified. Then, dissection proceeds between A9+10 and A6 along the intersegmental plane until V6 is exposed. The pulmonary ligament is incised up to the inferior pulmonary vein. The vein is cleared from surrounding tissue until V6 and the common basal vein are identified. The most important point is to clearly expose V6 keeping in mind that a tunnel will be created to separate S6 and S10.
The dissection continues in the fissure and the intersegmental plane between S6 and S10 is progressively made thinner. The intersegmental plane between S6 and S10 is initially divided by an endoscopic stapler to delimitate the superior and basal segments (Figure 1). Thus, a tunnel is created that first, connects the fissure with the posterior mediastinum, and second, that separates S6 and S10. The tunnel is divided by successive application of endoscopic staplers.
After the division of the intersegmental plane between S6 and S10, the branches of the pulmonary artery are easily recognized in the fissure (Video 2). A10 can be easily identified and divided using an endoscopic vascular stapler.
Once the segmental artery is cut, the bronchial branch B9+10 is identified posterior and cranial to the A10 stump. The posterior basal segmental bronchus (B10) is isolated and cut (Figure 2).
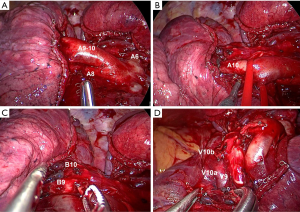
V10 is clearly identified once B10 has been divided. When the venous anatomy is not clear, it is preferable to divide only its lowermost tributary. As shown in the video, V9 is identified and kept, and then V10a and V10b are cut separately.
The division of the intersegmental plane is the most difficult as the intersegmental plane is tridimensional (Video 3). However, the tunneling technique facilitates completion of the intersegmental plane as S6 and S10 are already divided. The intersegmental plane is identified by using the systemic injection of indocyanine green with near-infrared imaging-system after transection of the segmental arteries. We use fluorescence with near infrared imaging (Karl Storz@, Germany). A total of 3 mL (2.5 mg/mL) of indocyanine green is injected through a peripheral venous line and demarcation line is promptly visualized between vascularized and devascularized lung parenchyma. Demarcation line (between the green enhanced parenchyma and normal parenchyma) is marked by electrocautery and the intersegmental plane between S10 and S9 is divided by successive application of endoscopic staplers. During this maneuver, it is important to include bronchovascular stumps in the specimen and to follow the division of the parenchyma in the direction of the segmental hilum.
The specimen is retrieved in a bag. Thereafter, a systematic lymph node dissection is performed. Finally, an intercostal block with local anesthesia (bupivacaine 0.5%) is applied between the 2nd and 8th intercostal space. A 28 French chest tube is introduced and the lung is re-expanded under direct vision.
Post-operative management
After initial transfer to the recovery room for 2 hours, the patient is transferred to the ward. The chest tube is removed in the absence of air leak and a 24-h serous output of less than 400 mL. In this patient, the chest tube was removed on postoperative day 1 and the patient was discharged on day 3.
Tips, tricks and pitfalls
Steps to intersegmental tunneling:
- Dissection of the major fissure;
- Identification of the common trunk for A9+10 and A6;
- Identification of V6 which delimitates the intersegmental plane between S6 and S10;
- Dissection of lymph node facilitates the exposure of the segmental bronchus;
- Division of A10, followed by B10 and V10;
- Systemic injection of indocyanine green with near-infrared imaging system more appropriate to identify the intersegmental plane between S10 and S9.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats-20-41). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Handa Y, Tsutani Y, Mimae T, et al. Surgical Outcomes of Complex Versus Simple Segmentectomy for Stage I Non-Small Cell Lung Cancer. Ann Thorac Surg 2019;107:1032-9. [Crossref] [PubMed]
- Sato M, Murayama T, Nakajima J. Thoracoscopic stapler-based “bidirectional” segmentectomy for posterior basal segment (S10) and its variants. J Thorac Dis 2018;10:S1179-86. [Crossref] [PubMed]
- Abdelsattar ZM, Blackmon SH. Using novel technology to augment complex video-assisted thoracoscopic single basilar segmentectomy. J Thorac Dis 2018;10:S1168-78. [Crossref] [PubMed]
- Karenovics W, Gonzalez M. How to decrease technical obstacles to difficult video-assisted thoracoscopic surgery segmentectomy? J Thorac Dis 2019;11:53-6. [Crossref] [PubMed]
- Bédat B, Abdelnour-Berchtold E, Krueger T, et al. Clinical outcome and risk factors for complications after pulmonary segmentectomy by video-assisted thoracoscopic surgery: Results of an initial experience. J Thorac Dis 2018;10:5023-9. [Crossref] [PubMed]
- Bédat B, Abdelnour-Berchtold E, Krueger T, et al. Impact of complex segmentectomies by video-assisted thoracic surgery on peri-operative outcomes. J Thorac Dis 2019;11:4109-18. [Crossref] [PubMed]
- Nakayama T, Kohno M, Izumi Y, et al. Innovative segmentectomy to remove the posterior segment of the lower lobe (S10) of the lung. Surg Today 2012;42:104-6. [Crossref] [PubMed]
Cite this article as: Ojanguren A, Sauvain MO, Forster C, Gonzalez M. Uniportal S10 segmentectomy by transfissural intersegmental tunneling. Video-assist Thorac Surg 2020;5:29.


