Cross-sectional survey on Chinese surgeons’ practice patterns and views on video-assisted thoracoscopic surgery
Introduction
Since the early 1990s, video-assisted thoracoscopic surgery (VATS) has been widely adopted to diagnose and treat diseases in the chest, such as spontaneous pneumothorax and lung cancer, especially the stage I and II non-small cell lung cancer (1). Substantially improved optical and surgical equipment and better anesthesia partially contribute to the widespread of VATS in recent years (2). Numerous previous studies have shown that VATS is as safe as open procedures and is associated with substantial benefits over open procedures in terms of simpler perioperative management, faster patient recovery, and better cost effectiveness (3-7). In particular, compared with open procedures, VATS can shorten the length of hospital stay, reduce intraoperative blood loss and the need of blood transfusion, decrease the incidence of surgical site infection, shorten the duration of chest tube drainage, and reduce postoperative pain (3-7).
VATS was introduced to China almost three decades ago (8). Although large scale multi-center studies to compare the clinical and health economic outcomes of VATS versus open procedures in Chinese patients are still lacking, single-center investigations with a relatively small sample size have shown an equal safety and surgical effectiveness of VATS and open procedures (9-11). VATS adoption rate in Chinese surgeons and hospitals remains unknown. Surgeons’ opinions could influence VATS adoption. To understand Chinese surgeons’ views on VATS and their VATS practice patterns, we developed a questionnaire to collect and analyze their opinions on the benefits of VATS over open procedures, the potential obstacles to adopt VATS, and the possible indications and contraindications of VATS to treat lung cancer. The current study may shed light on strategies to increase VATS adoption.
Methods
Participants
All Chinese surgeons attending the 5th Asian Masters of Minimally Invasive Thoracic Surgery event on June 3rd–4th, 2017 could participate. The event aimed to engage Chinese surgeons to discuss the technique of challenging minimally invasive procedures and to share experience in difficult surgical cases with international experts. A survey questionnaire was provided to attendees at on-site meeting registration on June 2nd, 2017. Attendees completed the questionnaire either at the on-site registration or on their convenient time during the event.
Questionnaire
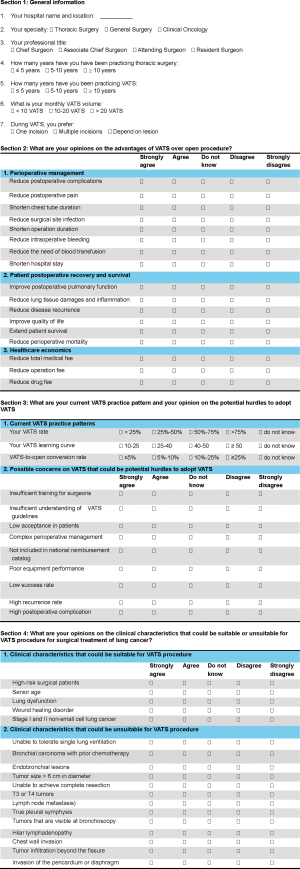
The survey questionnaire included four sections: (I) general information; (II) opinions on the advantages of VATS over open procedure; (III) VATS practice pattern and opinions on potential hurdles to adopt VATS; (IV) opinions on possible indications and contraindications of VATS to treat lung cancer. The survey was anonymous. Each section contained 7–20 questions. The questions in the general information section were to collect participants’ practice geographic location, professional title, experiences in thoracic surgery and VATS, and monthly VATS volume. Seventeen questions were used to collect participants’ opinions on the advantages of VATS over open procedures in terms of perioperative management, postoperative patient recovery, and healthcare economics. The questions on VATS practice patterns included the proportion of VATS, learning curve, and VATS-to-open conversion rate. The questionnaire also collected participants’ opinions on 7 possible concerns regarding VATS that could inhibit VATS adoption. In the last section of the questionnaire, opinions on possible indications and contraindications of VATS to treat lung cancer were collected. Incomplete questionnaires were excluded from data analysis. The survey questionnaire is presented in the supplementary file (Figure S1).
Statistical analysis
Categorical data are presented as percentage and number of cases. The statistical analysis software SPSS v21.0 was used. Chi-square test was used to compare the proportions of surgeons with different professional titles. P<0.05 was considered significantly different.
Results
General information
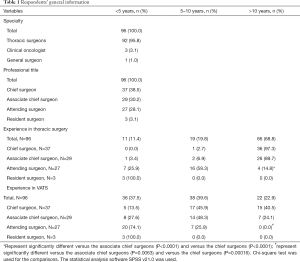
A total of 96 Chinese surgeons from ≥75 hospitals in ≥23 provinces completed the survey questionnaire. Of them, the majority (95.8%, 92/96) were thoracic surgeons; 3 (3.1%, 3/96) were clinical oncologists; only one (1.0%, 1/96) was a general surgeon (Table 1). Their professional titles were chief surgeons (38.5%, 37/96), associate chief surgeons (30.2%, 29/96), attending surgeons (28.1%, 27/96), and resident surgeons (3.1%, 3/96). Consistent with their professional titles, 97.3% of the chief surgeons and 89.7% of the associate chief surgeons had >10 years of experience in thoracic surgery, whereas only 14.8% of the attending surgeons had such long experience (P<0.0001 vs. the chief and vs. the associate chief surgeons, Table 1). Similar to their experience in thoracic surgery, significantly greater proportions of the chief surgeons (40.5%) and associate chief surgeons (24.1%) than the attending surgeons (0.0%, all P<0.05) had >10 years of experience in VATS (Table 1). The majority of the attending surgeons (74.0%) had performed VATS for <5 years (Table 1). Notably, higher percentage of the chief surgeons (40.5%) than the associate chief surgeons (24.1%) had >10 years of experience in VATS (Table 1). These results indicate that a senior professional title appears to be associated with longer years of experiences in VATS.
Full table
VATS practice patterns
Of the chief surgeons and associate chief surgeons, 45.9% and 44.8%, respectively, answered that they performed >20 VATS procedures per month, whereas only 14.8% of the attending surgeons answered such a monthly VATS volume (P=0.0088 vs. the chief and P=0.0147 vs. the associate chief surgeons) and most of them (70.3%) had <10 VATS procedures per month (Table 2). Although the attending surgeons answered a lower VATS volume, the proportion of VATS in their practice was high. Of the attending surgeons, 55.6% answered a proportion of VATS >75% in their practice; the proportion was similar to that of the associate chief surgeons (55.2%) but was higher than that of the chief surgeons (32.4%, P=0.064 vs. the attending surgeons) (Table 2). The attending surgeons appeared to believe they could learn VATS quickly. Compare to only 13.5% of the chief surgeons answering a learning curve of 10-25 VATS procedures, 25.9% of the attending surgeons believed their VATS skill could become stable after 10–25 VATS procedures (Table 2). Most of the participants (84.4%) answered that their VATS-to-open conversion rate was <10% (Table 2). Higher proportions of the chief surgeons (10.8%) and associate chief surgeons (6.9%) than the attending surgeons (0.0%, P=0.0776 vs. the chief surgeons) answered a VATS-to-open conversion rate of >10% in their practice (Table 2). Most of the 96 surgeons (81.3%) preferred either multiple incisions or determining the number of incisions based on lesion characteristics (Table 2). Only 10.8% of the chief surgeons used one incision in VATS, whereas higher proportions of associate chief surgeons (27.6%) and attending surgeons (18.5%) used one incision in VATS (Table 2).
Full table
Opinions on the benefits of VATS and potential hurdles to adopt VATS
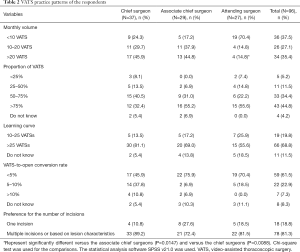
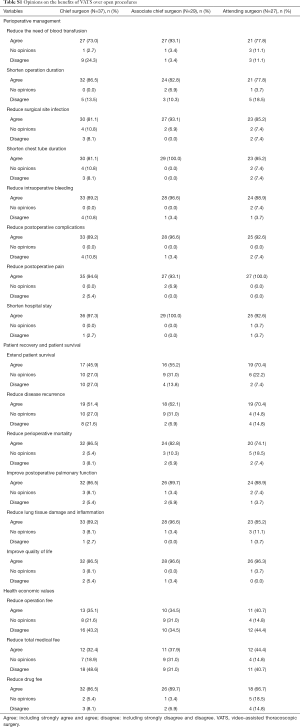
The 96 surgeons’ opinions on the advantages of VATS over open procedures in perioperative management appeared quite consistent (Figure 1A). The top four mostly agreed VATS benefits in perioperative management were shortening hospital stay (96.9%), reducing postoperative pain (95.8%), reducing postoperative complications (92.7%), and reducing intraoperative bleeding (91.7%) (Figure 1A). The majority of the surgeons also strongly agreed or agreed that VATS could shorten chest tube duration (88.5%), reduce surgical site infection (86.5%), shorten operation duration (83.3%), and reduce the need of blood transfusion (81.3%) (Figure 1A). Most of the surgeons also strongly agreed or agreed that VATS could improve postoperative patient recovery compared with open procedures (Figure 1B), such as improving quality of life (92.7%), reducing lung tissue damage and inflammation (90.6%), improving postoperative pulmonary function (88.5%), and reducing perioperative mortality (82.3%). However, relatively lower proportions strongly agreed or agreed that VATS could reduce disease recurrence (61.5%) and extend patient survival (57.3%) compared with open procedures (Figure 1B). The participants’ opinions on economic advantages of VATS over open procedures varied greatly. Although most of the 96 surgeons (81%) strongly agreed or agreed that VATS could reduce drug fee, large proportions of them disagreed that VATS could reduce total medical fee (40%) and operation fee (39%) (Figure 1C). The surgeons’ opinions on the advantages of VATS over open procedures were similar across the three professional titles (Table S1).
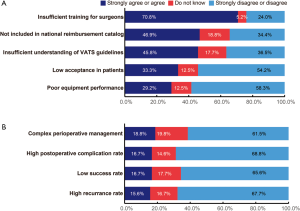
The mostly agreed potential hurdle to adopt VATS was insufficient training for surgeons (70.8%, Figure 2A). Less than 50% of the 96 surgeons strongly agreed or agreed that not-being included in the national reimbursement catalog and insufficient understanding of VATS guidelines could be potential hurdles (Figure 2A). The majority of the participants strongly disagreed or disagreed that low acceptance in patients (54.2%, Figure 2A) and poor equipment performance (58.3%, Figure 2A) could be hurdles to adopt VATS. In addition, the majority of the surgeons strongly disagreed or disagreed that potential concerns associated with VATS procedures or disease, such as complex perioperative management (61.5%), high postoperative complication rate (68.8%), low success rate (65.6%), and high recurrence rate (67.7%) could be potential hurdles to adopt VATS (Figure 2B). These opinions were similar in the chief surgeons, associate chief surgeons, and attending surgeons (Table S2).
Opinions on the indications and contraindications of VATS to treat lung cancer
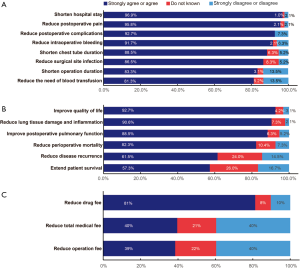
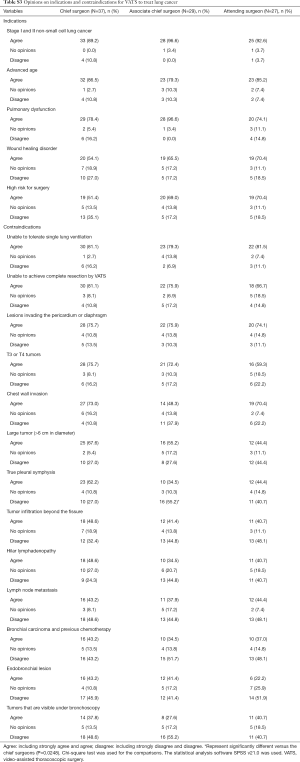
Most of the 96 participants strongly agreed or agreed that VATS should be performed on lung cancer patients with stage I and II non-small cell lung cancer (91.7%), advanced age (83.3%), or/and pulmonary dysfunction (82.3%) (Figure 3A), and 62.5% agreed that patients with wound healing disorder or/and high risk for surgery may be suitable for VATS (Figure 3A). The top 4 mostly agreed possible contraindications of VATS were being unable to tolerate single lung ventilation (80.2%), unable to achieve complete resection by VATS (75.0%), lesions invading the pericardium or diaphragm (74.0%), and T3 or T4 tumors (68.8%) (Figure 3B). For technically challenging lesions such as chest wall invasion and large tumor (>6 cm in diameter), 57.3–64.6% of the participants agreed that VATS may not be suitable (Figure 3B). Notably, <50% of the surgeon strongly agreed or agreed the following possible contraindications of VATS: true pleural symphysis (49.0%), tumor infiltration beyond the fissure (43.8%), hilar lymphadenopathy (42.7%), lymph node metastasis (41.7%), bronchial carcinoma and previous chemotherapy (38.5%), endobronchial lesion (37.5%), and tumors that are visible under bronchoscopy (36.5%) (Figure 3B). These results indicate Chinese surgeons’ views on possible contraindications of VATS appear very diverse.
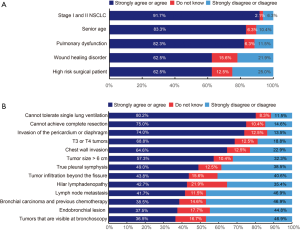
The surgeons with different professional titles shared similar opinions on most of the possible indications and contraindications of VATS. However, more associate chief surgeons (69.0%) and attending surgeons (70.4%) than the chief surgeons (51.4%) strongly agreed or agreed that VATS could be performed on patients with high surgical risk (Table S3). This result indicates that young surgeons may be less conservative on the possible indications of VATS compared with senior ones. In addition, more attending surgeons (44.4%) than chief surgeons (27.0%) and associate chief surgeons (27.6%) disagreed that a tumor with a diameter >6 cm should be a contraindication. Furthermore, more associate chief surgeons (55.2%, P=0.0248 vs. chief surgeons) and attending surgeons (40.7%) than the chief surgeons (27.0%) disagreed that true pleural symphysis should be a contraindication. Similarly, greater percentages of the associate chief surgeons (44.8%) and the attending surgeons (40.7%) than the chief surgeons (24.3%) disagreed that hilar lymphadenopathy could be a contraindication (Table S3). These findings suggest that Chinese thoracic surgeons at the junior or middle career levels appear more likely to perform VATS on anatomically and/or clinically challenging cases than senior surgeons.
Discussion
The current study collected 96 Chinese surgeons’ practice patterns and opinions on VATS. The 96 surgeons were from all the 6 geographic regions (North, Northeast, East, South Central, Southwest, and Northwest) in China and across all of the 3 professional titles (chief, associate chief, and attending surgeons) of thoracic surgery. Each of the 3 professional titles included approximately one third of the 96 surgeons. Thus, their opinions may more likely reflect the views of whole Chinese thoracic surgeon community rather than the opinions of thoracic surgeons at a certain professional level.
The surgeons’ experiences in VATS were consistent with their professional titles. The chief and associate chief surgeons had performed VATS for significantly longer years and had significantly higher monthly volume than the attending surgeons, indicating that the surgeons’ answers to the questionnaire may be reliable. Notable, although most of the attending surgeons (junior surgeons) had <5 years of experience in VATS and <10 VATS procedures per month, the percentage of them (55.6%) answering a proportion of VATS >75% was as high as the associate chief surgeons (55.2%) and even higher than the chief surgeons (32.4%). These findings suggest that Chinese young thoracic surgeons appear more likely to perform VATS than established surgeons. In addition, our study also indicated that Chinese young thoracic surgeons seem very confident in performing VATS because more attending surgeons answered a short learning curve (10–25 VATS procedures) and fewer of them answered a >10% VATS-to-open conversion rate compared with the senior and established surgeons (chief and associate chief surgeons). Furthermore, the result showing a higher proportion of the attending surgeons (18.5%) than the chief surgeons (10.8%) choosing one portal VATS support that Chinese young thoracic surgeons may be more likely adopt new VATS technique.
Our survey found that the benefits of VATS over open procedures in perioperative management and patient recovery were uniformly agreed in the 96 participants (81.3–96.9% agreement rate). These benefits of VATS are consistently supported by the results from numerous previous studies (3-7). However, the 96 surgeons’ opinions on the economic benefits of VATS appear different from the findings of previous studies that were conducted in other countries. In this survey, although the majority of the 96 surgeons (81.0%) agreed that VATS could reduce drug fee, most of them disagreed that VATS might reduce total medical fee and operation fee. In contrast, previous studies conducted in US and Europe consistently support that VATS lung resection is associated with lower total hospital cost compared with open procedures (12-15). Similar to the opinions of the current survey on total medical fee, in a single-center retrospective observational study, Li and colleagues found significantly increased total hospital cost of VATS compared with open lobectomy in China (10). Therefore, VATS may be associated with higher total hospital and operation costs in China but lower in US and Europe. The opposite effects of VATS on the medical costs in China and US may be explained by the very different national pricing and reimbursement policies for healthcare in the two countries. For example, the fees for surgeons and other health care professionals are much lower in China than in US, whereas the fees for VATS equipment and supplies are substantially higher in China. Although VATS may cause higher total hospital and operation costs than open procedures in China, VATS could be associated with better cost-effectiveness than open procedures when the VATS-associated clinical benefits were considered.
In our survey, insufficient training for surgeons was the mostly agreed potential obstacle to adopt VATS, whereas all of the other possible concerns on VATS that could discourage VATS adoption were disagreed by most of the participants. Thus, based on Chinese thoracic surgeons’ opinion, VATS may be commonly accepted by patients although VATS could be more expensive than open procedures and VATS appears not technically too challenging to be operated. Similar to our study, Cao and colleagues conducted a cross-sectional survey on lobectomy approach (X-SOLA study) (16). In the X-SOLA study, Cao and colleagues investigated the attitudes of 838 thoracic surgeons worldwide toward VATS lobectomy and found that a need for VATS lobectomy training was agreed by both the surgeons who only performed open lobectomy and the surgeons who only perform VATS lobectomy (16).
Our survey showed that stage I and II NSCLC was the mostly agreed indication for VATS, suggesting that Chinese thoracic surgeons’ opinions on the indications for VATS appear to be consistent with the international guidelines on VATS (17,18), which recommend VATS for patients with stage I and II non-small cell lung cancer. Inability to tolerate single lung ventilation, inability to achieve complete resection, and T3 or T4 tumors have been considered as absolute contraindication to VATS lobectomy (19). Our survey showed that these contraindications were also agreed widely in the Chinese surgeons. In contrast to the more consistent views on clinical benefits of VATS, such as the benefits in perioperative management and postoperative recovery, the survey respondents’ views on the contraindications of VATS were less consistent and varied widely, particularly on anatomically and/or clinically challenging cases. Notably, our results showed that more attending surgeons than the well-established surgeons (chief surgeons) did not consider challenging clinical and tumor characteristics, such as large tumors with a diameter >6 cm, true pleural symphysis, and hilar lymphadenopathy, as contraindications of VATS to treat lung cancer. These data indicate that junior Chinese thoracic surgeons may hold less conservative views toward VATS and appear more likely to perform VATS on anatomically and/or clinically challenging cases than senior surgeons. These attending surgeons’ views on less strict contraindications may also reflect the evolution of indications and contraindications of VATS. As the equipment and technique of VATS advance continuously, one would expect that the contraindications of VATS will be increasingly narrowed. Thus, the results of this survey suggest that Chinese thoracic surgeons might not reach a consensus on contraindications of VATS.
The limitation of this study is that the number of respondent is relatively small. Nevertheless, the practice locations of the 96 surgeons were cross the entire country and the 96 surgeons were distributed evenly at the three professional titles. Thus, their opinions may be representative among Chinese thoracic surgeons. These opinions are subjective. Objective clinical investigations are required to confirm the findings. Moreover, although the current study only collected opinions of Chinese surgeons, the findings could shed light on the strategies to improve VATS adoption.
Conclusions
The benefits of VATS over open procedures in perioperative management and patient recovery were commonly agreed in Chinese thoracic surgeons. Chinese thoracic surgeons also consistently agreed on the early stage lung cancer as the indication of VATS. Insufficient training may be a potential obstacle to adopt VATS. Training workshops may broaden VATS adoption.
Full table

Full table
Full table
Acknowledgments
The authors greatly appreciate Mr. Santosh Agarwal for providing insightful comments to improve the manuscript. The authors also thank Ms. Lydia Wang for collecting completed questionnaires and Mr. Shijun Yu for his constructive comments on the questionnaire design.
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2018.10.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Onugha O, Ivey R, McKenna R. Novel Techniques and Approaches to Minimally Invasive Thoracic Surgery. Surg Technol Int 2017;30:231-5. [PubMed]
- Mohiuddin K, Swanson SJ. Maximizing the benefit of minimally invasive surgery. J Surg Oncol 2013;108:315-9. [Crossref] [PubMed]
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [Crossref] [PubMed]
- Chen FF, Zhang D, Wang YL, et al. Video-assisted thoracoscopic surgery lobectomy versus open lobectomy in patients with clinical stage I non-small cell lung cancer: a meta-analysis. Eur J Surg Oncol 2013;39:957-63. [Crossref] [PubMed]
- Laursen LØ, Petersen RH, Hansen HJ, et al. Video-assisted thoracoscopic surgery lobectomy for lung cancer is associated with a lower 30-day morbidity compared with lobectomy by thoracotomy. Eur J Cardiothorac Surg 2016;49:870-5. [Crossref] [PubMed]
- Falcoz PE, Puyraveau M, Thomas PA, et al. Video-assisted thoracoscopic surgery versus open lobectomy for primary non-small-cell lung cancer: a propensity-matched analysis of outcome from the European Society of Thoracic Surgeon database. Eur J Cardiothorac Surg 2016;49:602-9. [Crossref] [PubMed]
- Chen QK, Chen C, Chen XF, et al. Video-assisted thoracic surgery for pulmonary aspergilloma: a safe and effective procedure. Ann Thorac Surg 2014;97:218-23. [Crossref] [PubMed]
- Heng Z. Brief History of Video-assisted Thoracic Surgery in China. Chinese Journal of Minimally Invasive Surgery 2011;11:295-7.
- Yang X, Wang S, Qu J. Video-assisted thoracic surgery (VATS) compares favorably with thoracotomy for the treatment of lung cancer: a five-year outcome comparison. World J Surg 2009;33:1857-61. [Crossref] [PubMed]
- Li Y, Wang J. Comparison of clinical outcomes for patients with clinical N0 and pathologic N2 non-small cell lung cancer after thoracoscopic lobectomy and open lobectomy: a retrospective analysis of 76 patients. J Surg Oncol 2012;106:431-5. [Crossref] [PubMed]
- Zhong C, Yao F, Zhao H. Clinical outcomes of thoracoscopic lobectomy for patients with clinical N0 and pathologic N2 non-small cell lung cancer. Ann Thorac Surg 2013;95:987-92. [Crossref] [PubMed]
- Farjah F, Backhus LM, Varghese TK, et al. Ninety-day costs of video-assisted thoracic surgery versus open lobectomy for lung cancer. Ann Thorac Surg 2014;98:191-6. [Crossref] [PubMed]
- Howington JA, Gunnarsson CL, Maddaus MA, et al. In-hospital clinical and economic consequences of pulmonary wedge resections for cancer using video-assisted thoracoscopic techniques vs traditional open resections: a retrospective database analysis. Chest 2012;141:429-35. [Crossref] [PubMed]
- Swanson SJ, Meyers BF, Gunnarsson CL, et al. Video-assisted thoracoscopic lobectomy is less costly and morbid than open lobectomy: a retrospective multiinstitutional database analysis. Ann Thorac Surg 2012;93:1027-32. [Crossref] [PubMed]
- Ramos R, Masuet C, Gossot D. Lobectomy for early-stage lung carcinoma: a cost analysis of full thoracoscopy versus posterolateral thoracotomy. Surg Endosc 2012;26:431-7. [Crossref] [PubMed]
- Cao C, Tian DH, Wolak K, et al. Cross-sectional survey on lobectomy approach (X-SOLA). Chest 2014;146:292-8. [Crossref] [PubMed]
- Howington JA, Blum MG, Chang AC, et al. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e278S-e313S.
- Yamashita S, Goto T, Mori T, et al. Video-assisted thoracic surgery for lung cancer: republication of a systematic review and a proposal by the guidelines committee of the Japanese Association for Chest Surgery 2014. Gen Thorac Cardiovasc Surg 2014;62:701-5. [Crossref] [PubMed]
- Hanna JM, Berry MF, D'Amico TA. Contraindications of video-assisted thoracoscopic surgical lobectomy and determinants of conversion to open. J Thorac Dis 2013;5:S182-9. [PubMed]
Cite this article as: Su G, Cai L. Cross-sectional survey on Chinese surgeons’ practice patterns and views on video-assisted thoracoscopic surgery. Video-assist Thorac Surg 2018;3:43.