
Virtual simulation and learning new skills in video-assisted thoracic surgery
Introduction
Traditionally, thoracic surgery operations have been performed by thoracotomy. Over the last decade, video-assisted thoracic surgery (VATS) has changed the treatment of patients with lung diseases, in particular, patients with lung cancer (1). In many cases, in fact, it is possible to perform oncologic therapeutic procedures like lobectomies by VATS, even in the case of extensive disease (2). Multiple or single port can perform the VATS approach. The adoption of this technique has proven to give better results, providing a faster postoperative recovery, less pain and fewer complications (3,4). Therefore, the number of patients operated by VATS is rapidly increasing, along with the need for proper training for surgeons in this technique. The effectiveness of training VATS resident surgeons using virtual reality (VR) simulators is stated in many studies, however its use is still not established in the normal practice (5). Useful VR simulators can integrate 3-dimensional (3D) imaging, have customizable instrumentation and should expose trainees to many anatomic variations to reduce the need for continuous one-on-one instructor observation (6,7). The purpose of this study is to create a VR curriculum to offer an evidence-based approach for VATS training programs.
Methods
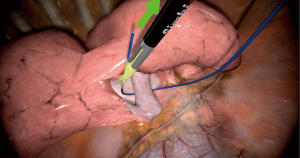
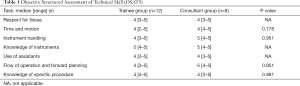
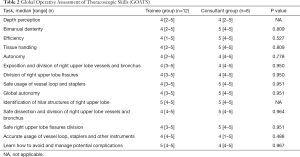
Each participant has been given time with an experienced operator to familiarize with the simulator before starting the assignments. To begin with, every task was demonstrated through the experienced surgeon and the participants had the chance to ask questions. No assistance has been given during hands-on training. Data for each performed assignment has been registered instantly and objectively by the simulator. Data include many information, like the time taken to execute the task, the economy of movement and error scores. The simulator software recorded the data. Basic skills were evaluated with two tests. The Objective Structured Assessment of Technical Skill (OSATS) developed two scores: an operation-specific checklist and a detailed global rating scale. In this assessment, the checklists have been assessed as simply “done correctly or not”, and the global performance level will be a 5-point, anchored Likert scale (Table S1) (8). The other test was the Global Operative Assessment of Thoracoscopic Skills (GOATS) derived from Global Operative Assessment of Laparoscopic Skills, used to evaluate the performance of laparoscopic surgeons. This was based on the concept that the performance can be assessed in several categories (called domains) such as depth perception, bimanual dexterity, efficiency, tissue handling, autonomy, and level of difficulty. Each area was scored from 1 to 5 using a global rating scale and a task-specific checklist. This method constructed validity for the assessment of surgeons’ performance of the entire VATS procedure rather than for just a few steps (Table S2) (9). On completing the operation, surgeons were evaluated for the cognitive workload according to the National Aeronautics Space Administration-Task Load Index (NASA-TLX), a widely recognized tool for self-reporting workload perception. The cognitive workload is a hypothetical construct that represents the cost incurred by a human operator to achieve a particular level of performance. Because the definition of the cognitive workload is human centred rather than task centred, the cognitive workload is defined uniquely by the demands of an objective task: as such, it reflects multiple attributes that may have different relevance for different individuals. The NASA-TLX rating scale is a multidimensional assessment tool that allows participants to rate their cognitive workloads on six scales (Table S3): mental demand, physical demand, temporal demand, effort, performance and frustration during task execution (10). A comprehensive evaluation questionnaire was also requested (Table S4). A 3D Systems/Simbionix simulator reproducing a right upper lobectomy (Littleton, Colorado, USA) was used from the voluntaries to complete the tasks (Figures 1-3).

Statistical analysis
A power calculation determined the sample size. Previous data in the literature helped us predicting the difference that we would observe in laparoscopy and robotics, so we adapted this data for VATS. Using an α value of 0.05, a β value of 0.2, and a δ value of 1.5 standard deviations, the power calculation yielded a group size of 26 subjects who will be stratified by year of training and compared with data from a cohort of “skilled” surgeons. Fisher’s exact test was used to compare differences in categorical variables and the Wilcoxon rank sum test for continuous variables. Differences in performance between groups were analysed by use of the Kruskal-Wallis test for nonparametric data. The NASA-TLX consists of two parts: ratings and weights Ratings for each of the six subscales will be obtained from the subjects following the completion of a task. Weights were determined by the subjects’ choices of the subscale most relevant to the workload for them from a pair of options. The heights were calculated from the tally of these options from 15 combinatorial pairs created from the six subscales. The ratings and weights will then be combined to compute a weighted average for an overall workload score.
Results
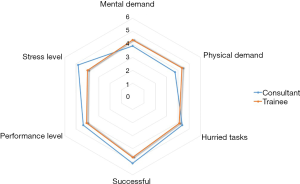
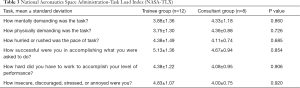
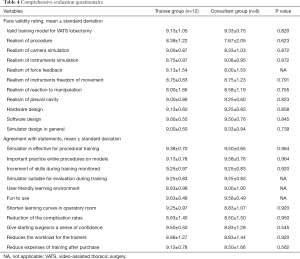
Twenty voluntaries completed all tasks (trainees =12, consultants =8). Comparisons between novice and experienced groups showed that all tests yielded similar results on P values. In particular, OSATS (Table 1) and GOATS (Table 2) performance of both groups were similar without skills differences regarding experience. The performance was similar between two groups. Median scores of consultants were taken as benchmark levels. Comparison of the trainees’ scores with benchmark levels showed that all participants could accomplish the set criteria. The Kiviat diagram of the NASA-TLX cognitive workload assessment showed a greater mental and physical demand in the trainee group; in the consultant group, the stress and performance level were greater than in the trainee group (Figure 4). Nevertheless, these differences between groups were not significantly different (Table 3). Comprehensive evaluation questionnaire showed no significant differences between trainee and consultant groups (Table 4).
Full table
Full table
Full table
Full table
Discussion
The traditional training model of modern thoracic surgical education is evolving in relation to patient safety, increasing the difficulty and heterogeneity of the surgical procedures. Recent analyses state that, by complex VATS procedures, 90 to 100 cases may be required to achieve an optimal technical level (shorter operative time and lower conversion rate (13,14). To adapt to these factors, a development of the actual teaching programs is taking place to advance cognitive and procedural abilities prior to performing in the operation theater. VR training programs are not designed as an alternative to the practice in operating theatres, but it should support a portion of the learning curve. The best approach for VR training and assessment is still debated and investigated. VR simulators have many advantages over animal models or over the traditional box trainer, including a shorter preparation time or more realistic features of the simulated VATS procedures. A VR simulator can, in fact, realistically simulate complications like bleedings or anatomical variations, which are very useful tools to speed up the learning curve for VATS procedures. Furthermore, VR simulators intended to stimulate both cognitive and psychomotor resources offer a fundamental support for practical training and evaluation. The interaction of the cognitive and psychomotor layers in simulations has been demonstrated to enhance the learning process (15). The amount of training with a VR simulator is unrestricted, and the expense for each surgery is affordable, after purchasing the simulator. Performance evaluation can be employed for appraisal and credential. This should improve patient safety, as the resident is already confident with the procedures (16). Certainly, developing a VR simulator is expensive and so it is necessary for VR trainings to be part of the surgeons’ education throughout their career, so that the simulator’s expenses can be compensated (17).
Many studies already published in the literature about VR simulators for laparoscopic training state the impact of this sort of training on the performance in vivo. In a randomized controlled trial of VR laparoscopy training performed from Meyerson et al., the performance level of junior residents was comparable to that of intermediately experienced laparoscopists. Operation time was halved (18).
Seymour et al. state that the use of VR simulation significantly developed a high level of performance of trainees in the operating room during laparoscopic cholecystectomy (19). Regarding the thoracic surgery training, our study clearly supports the inclusion of VR simulation into surgical training programs and other studies in the literature support this statement. For instance, Solomon et al. assessed the residents on a VATS right upper lobectomy employing a dedicated simulator for lung resections. They validated that VR cognitive task simulation could overcome the deficiencies of existing training models (6).
Altogether, different VR simulators with various features are on the market currently and only a few of them have been officially evaluated regarding their teaching effectiveness (20). Particularly for the thoracic surgery, there is currently a predominance of models simulating bronchoscopy but a lack of simulators of thoracoscopic procedures, so the research for the perfect simulator is not ended, yet.

Full table

Full table

Full table

Full table
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Yoshihisa Shimada) for the series “Current Status of Surgical Simulation in Video-assisted Thoracic Surgery and Robot-assisted Thoracic Surgery” published in Video-Assisted Thoracic Surgery. The article has undergone external peer review.
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2018.08.03). The series “Current Status of Surgical Simulation in Video-assisted Thoracic Surgery and Robot-assisted Thoracic Surgery” was commissioned by the editorial office without any funding or sponsorship. LB serves as an unpaid editorial board member of Video-Assisted Thoracic Surgery from Jul 2016 to May 2019. MS serves as an unpaid editorial board member of Video-Assisted Thoracic Surgery from Mar 2017 to May 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shah RD, D'Amico TA. Modern impact of video assisted thoracic surgery. J Thorac Dis 2014;6:S631-6. [PubMed]
- Sekhniaidze D, Gonzalez-Rivas D. Uniportal video-assisted thoracoscopic sleeve resection. Ann Cardiothorac Surg 2016;5:145-6. [Crossref] [PubMed]
- Vannucci F, Gonzalez-Rivas D. Is VATS lobectomy standard of care for operable non-small cell lung cancer? Lung Cancer 2016;100:114-9. [Crossref] [PubMed]
- Bedetti B, Scarci M, Gonzalez-Rivas D. Technical steps in single port video-assisted thoracoscopic surgery lobectomy. J Vis Surg 2016;2:45. [Crossref] [PubMed]
- Jensen K, Bjerrum F, Hansen HJ, et al. A new possibility in thoracoscopic virtual reality simulation training: development and testing of a novel virtual reality simulator for video-assisted thoracoscopic surgery lobectomy. Interact Cardiovasc Thorac Surg 2015;21:420-6. [Crossref] [PubMed]
- Solomon B, Bizekis C, Dellis SL, et al. Simulating video-assisted thoracoscopic lobectomy: a virtual reality cognitive task simulation. J Thorac Cardiovasc Surg 2011;141:249-55. [Crossref] [PubMed]
- Aggarwal R, Crochet P, Dias A, et al. Development of a virtual reality training curriculum for laparoscopic cholecystectomy. Br J Surg 2009;96:1086-93. [Crossref] [PubMed]
- Reznick RK. Teaching and testing technical skills. Am J Surg 1993;165:358-61. [Crossref] [PubMed]
- Vassiliou MC, Feldman LS, Andrew CG, et al. A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg 2005;190:107-13. [Crossref] [PubMed]
- Cao A, Chintamani KK, Pandya AK, et al. NASA TLX: software for assessing subjective mental workload. Behav Res Methods 2009;41:113-7. [Crossref] [PubMed]
- Bedetti B, Bertolaccini L, Patrini D, et al. Virtual reality (VR) simulator of a right video-assisted thoracic surgery (VATS) upper lobectomy. Asvide 2018;5:713. Available online: http://www.asvide.com/article/view/26669
- Bedetti B, Bertolaccini L, Patrini D, et al. Haemorrhagic complication during a simulation of a right video-assisted thoracic surgery (VATS) upper lobectomy. Asvide 2018;5:714. Available online: http://www.asvide.com/article/view/26670
- Mazzella A, Olland A, Falcoz PE, et al. Video-assisted thoracoscopic lobectomy: which is the learning curve of an experienced consultant? J Thorac Dis 2016;8:2444-53. [Crossref] [PubMed]
- Yang HC, Kim S, Yum S, et al. Learning curve of single-incision thoracoscopic surgery for primary spontaneous pneumothorax. Surg Endosc 2017;31:1680-7. [Crossref] [PubMed]
- Kahol K, Vankipuram M, Smith ML. Cognitive simulators for medical education and training. J Biomed Inform 2009;42:593-604. [Crossref] [PubMed]
- Petersen RH, Hansen HJ. Learning curve associated with VATS lobectomy. Ann Cardiothorac Surg 2012;1:47-50. [PubMed]
- Aggarwal R, Mytton OT, Derbrew M, et al. Training and simulation for patient safety. Qual Saf Health Care 2010;19:i34-43. [Crossref] [PubMed]
- Meyerson SL, LoCascio F, Balderson SS, et al. An inexpensive, reproducible tissue simulator for teaching thoracoscopic lobectomy. Ann Thorac Surg 2010;89:594-7. [Crossref] [PubMed]
- Seymour NE, Gallagher AG, Roman SA, et al. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 2002;236:458-63; discussion 463-4. [Crossref] [PubMed]
- Trehan K, Kemp CD, Yang SC. Simulation in cardiothoracic surgical training: where do we stand? J Thorac Cardiovasc Surg 2014;147:18-24.e2. [Crossref] [PubMed]
Cite this article as: Bedetti B, Bertolaccini L, Patrini D, Schmidt J, Scarci M. Virtual simulation and learning new skills in video-assisted thoracic surgery. Video-assist Thorac Surg 2018;3:35.


