
A natural way to extend the indications for video-assisted thoracoscopic surgery in patients with advanced lung cancer
Video-assisted thoracoscopic surgery (VATS) was first reported by Levi et al. in 1990 (1). VATS has become an attractive surgical procedure for benign diseases because of its low invasiveness (2,3). As experience performing VATS for benign diseases has accumulated, VATS has gradually begun to be used for lung cancer surgery. Since Roviaro et al. reported the first lobectomy using a videoendoscope for lung cancer, many investigators have used VATS for lung cancer operations and have reported the resulting outcomes (4). VATS is obviously superior to an open thoracotomy (Open) in terms of postoperative pain and cosmesis. However, the safety and adequacy of VATS for cancer operations needs to be confirmed.
VATS for early lung cancer
As the first step in applying VATS for lung cancer, VATS has been used in patients with an early disease stage. Two prospective randomized trials have compared VATS and Open in patients with stage I lung cancer, although the sizes of both trials were relatively small. Kirby et al. randomized 55 patients with stage I disease into two groups, a VATS lobectomy group and muscle-sparing lobectomy group, and compared the operative time, volume of bleeding, period of chest tube use, postoperative pain, period of hospital stay, and rate of postoperative complications. They reported that there were no significant differences between the two groups in terms of operative time, volume of bleeding, period of chest tube use, postoperative pain, or period of hospital stay, while more postoperative complications occurred in the muscle-sparing lobectomy group (24% in the VATS group and 53% in the muscle-sparing group, P<0.05) (5). Sugi et al. also conducted a similar randomized control study in 100 patients with stage IA NSCLC (6). They reported that there were no significant differences between the VATS group and the Open group with regard to the number of resected lymph nodes (21.2 in the VATS group and 21.8 in the Open group), the rate of recurrence (10% in VATS and 17% in Open), or the 5-year survival rate (90% in VATS and 85% in Open). They concluded that VATS with lymph node dissection enabled an excellent 5-year survival outcome comparable to that achieved in the Open group.
There are many observational cohort studies and several meta-analyses in patients with early lung cancer (Table 1). Yan et al. conducted a systemic review and meta-analysis comparing VATS and Open. They included two randomized studies described above and 19 observational cohort studies and evaluated the safety and efficacy of VATS in patients with stage I disease (7). They reported that there were no significant statistical differences between VATS and Open in terms of postoperative prolonged air leakage, arrhythmia, pneumonia, or mortality. On the other hand, VATS was superior in terms of the systemic recurrence rate (relative risk =0.57; 95% confidential interval, 0.34–0.95; P=0.03) and had an improved 5-year mortality rate (relative risk =0.72; 95% confidential interval, 0.45–0.97; P=0.04), while no difference in locoregional recurrence was seen. Taioli et al. conducted a meta-analysis that included 2,106 patients with VATS and 2,661 patients with Open from among 20 observational cohort studies and evaluated the 5-year survival (8). They demonstrated an advantage in long-term mortality for patients who underwent VATS, compared with the patients who underwent Open, although a large degree of heterogeneity existed among the studies. Cai et al. also conducted a meta-analysis comparing VATS and Open in patients with Stage I disease and reported that VATS was associated with a longer 5-year survival, higher local recurrence rate, similar distant recurrence rate and lower total complication rate, compared with Open (9). VATS was also associated with lower rates of arrhythmias, prolonged air leakage, and pneumonia, although the differences were not statistically significant. Three meta-analyses similarly concluded that VATS was superior to Open in terms of survival and was equivalent in terms of perioperative complications, but it should be noted that the papers to which the three meta-analyses referred mostly overlapped. It was, therefore, natural that the three meta-analyses reached similar conclusions.
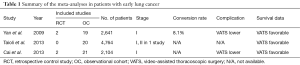
Full table
As described above, two RCTs and three meta-analyses evaluated VATS in early lung cancer, but the study sizes of the two RCTs were relatively small and the three meta-analyses utilized overlapping studies. Thus, it is difficult to make a clear conclusion with a high quality and high level of evidence based on these studies. A large multi-institutional prospective randomized-controlled trial would be optimal, but such a study comparing VATS vs. Open for lung cancer is unlikely to ever be completed, since the advantages of VATS, such as less pain and superior pulmonary function during the early postoperative phase, are already well known and VATS is now being performed in clinical practice (10). In this scenario, observational studies remain the most reliable source of scientific information. Under this circumstance and judging from the available data, it seems reasonable to accept that both the short-term and long-term outcomes of VATS for the treatment of early lung cancer might be equivalent to those of Open, making VATS a feasible alternative method.
VATS for advanced lung cancer
With the accumulation of experience performing VATS for early lung cancer, it was natural to expand the indications for VATS to advanced lung cancer as the next step. Several studies have addressed the feasibility of VATS for advanced lung cancer; three single arm observational cohort studies and four observational cohort studies comparing VATS and Open have been performed, but an RCT or meta-analysis comparing VATS and Open has not yet been done (Table 2). Huang et al. reported the outcomes of VATS following neoadjuvant chemotherapy in patients with stage II–IIIB disease (11). The perioperative complication rate was 9.5% and the mortality rate was 2.4%. They concluded that VATS following neoadjuvant chemotherapy was safe and feasible for the treatment of advanced lung cancer. Gonzales-Rivas et al. conducted a comparison of uniportal VATS between early lung cancer and advanced lung cancer (12). The median number of resected lymph nodes (14 for early lung cancer and 16 for advanced lung cancer) was significantly higher for the advanced cases, and the complication rate (17.2% for early lung cancer and 14% for advanced lung cancer) was similar in both groups. They concluded that uniportal VATS for advanced cases was as safe and feasible as that for early cases. Chen et al. conducted a comparison between VATS and Open in patients with stage II–IIIA disease (13). They included 250 patients with VATS and 161 patients with Open and compared the perioperative outcomes and survival. Furthermore, interestingly, they performed propensity-matched analysis in the selected 240 patients to remove patient bias. In total, 11.7% of the patients in the VATS group required a conversion to an open thoracotomy because of bleeding, a large tumor size, lymph node calcification, margins that needed to be extended, and failed fissure dissociation. The hospital stay in the VATS group was shorter than that in the Open group, while the number of resected lymph nodes and the perioperative complication rates were similar between the two groups. Disease-free survival and overall survival were also similar between the two groups. They concluded that VATS can be performed in most cases of advanced lung cancer without compromising the perioperative outcome or oncological efficacy.

Full table
The mean conversion rate of the seven studies evaluating VATS in advanced lung cancer was 10.6%, which is likely to be slightly higher than that for early-stage disease. This result is understandable because lymph node dissection in patients with N1 or N2 or vessel isolation in patients whose tumors are located close to a large vessel might be more difficult and might often require conversion to an open thoracotomy.
All seven studies supported that VATS for advanced lung cancer was feasible and equivalent to Open. However, it should be noted that a patient selection bias was likely present, since VATS was likely to be performed in patients who were expected to be capable of undergoing VATS and Open was likely to be performed in other patients and that this selection bias surely had favorable influence on the outcomes of VATS.
Decaluwe et al. evaluated intraoperative complications during VATS in 3,076 patients from six European centers (14). Conversion to Open was observed in 5.5% of the cases: 21.8% were for oncological reasons, 29.4% were for technical reasons, and 48.8% were for complications. Vascular injuries were reported in 2.9% of the patients. In 1.5%, major intraoperative complications were identified. These consisted of the erroneous transection of bronchovascular structures or injuries to gastrointestinal organs or the proximal airway. Twenty-three percent of the in-hospital mortalities were related to major intraoperative complications. Interestingly, the authors evaluated the correlation between the surgeon’s experience and the incidence of intraoperative complications and reported that surgeon experience was not correlated with the incidences of vascular injuries or major complications. Byun et al. also evaluated intraoperative complications and reported that the intraoperative complications and conversion to Open might be associated with postoperative respiratory complications (15). Once intraoperative complications occur during VATS, their repair can be difficult and time-consuming, and the risk of postoperative complications might increase. Thus, the decision to convert should be made promptly to reduce the potential risk of postoperative complications and to maintain curability, especially in patients with advanced lung cancer.
With the accumulation of further experience performing VATS, the indications for VATS have been extended to include advanced lung cancer. The outcomes of VATS in advanced cancer are likely to be comparable to those of Open in the selected patients. Patient selection and the timing of conversion to Open should be carefully and promptly decided, especially in patients with advanced lung cancer.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Dr. Liu Chengwu (Department of Thoracic Surgery, West China Hospital, Sichuan University, Chengdu, China).
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2017.06.04). The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Levi JF, Kleinmann P, Riquet M, et al. Percutaneous parietal pleurectomy for recurrent spontaneous pneumothorax. Lancet 1990;336:1577-8. [Crossref] [PubMed]
- Cole FH Jr, Cole FH, Khandekar A, et al. Video-assisted thoracic surgery: primary therapy for spontaneous pneumothorax? Ann Thorac Surg 1995;60:931-3; discussion 934-5. [Crossref] [PubMed]
- Sawada S, Watanabe Y, Moriyama S. Video-assisted thoracoscopic surgery for primary spontaneous pneumothorax: evaluation of indications and long-term outcome compared with conservative treatment and open thoracotomy. Chest 2005;127:2226-30. [Crossref] [PubMed]
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- Kirby TJ, Mack MJ, Landreneau RJ, et al. Lobectomy--video-assisted thoracic surgery versus muscle-sparing thoracotomy. A randomized trial. J Thorac Cardiovasc Surg 1995;109:997-1001; discussion 1001-2. [Crossref] [PubMed]
- Sugi K, Kaneda Y, Esato K. Video-assisted thoracoscopic lobectomy achieves a satisfactory long-term prognosis in patients with clinical stage IA lung cancer. World J Surg 2000;24:27-30; discussion 30-1. [Crossref] [PubMed]
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [Crossref] [PubMed]
- Taioli E, Lee DS, Lesser M, et al. Long-term survival in video-assisted thoracoscopic lobectomy vs open lobectomy in lung-cancer patients: a meta-analysis. Eur J Cardiothorac Surg 2013;44:591-7. [Crossref] [PubMed]
- Cai YX, Fu XN, Xu QZ, et al. Thoracoscopic lobectomy versus open lobectomy in stage I non-small cell lung cancer: a meta-analysis. PLoS One 2013;8:e82366 [Crossref] [PubMed]
- Nakata M, Saeki H, Yokoyama N, et al. Pulmonary function after lobectomy: video-assisted thoracic surgery versus thoracotomy. Ann Thorac Surg 2000;70:938-41. [Crossref] [PubMed]
- Huang J, Xu X, Chen H, et al. Feasibility of complete video-assisted thoracoscopic surgery following neoadjuvant therapy for locally advanced non-small cell lung cancer. J Thorac Dis 2013;5:S267-73. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- Chen K, Wang X, Yang F, et al. Propensity-matched comparison of video-assisted thoracoscopic with thoracotomy lobectomy for locally advanced non-small cell lung cancer. J Thorac Cardiovasc Surg 2017;153:967-976.e2. [Crossref] [PubMed]
- Decaluwe H, Petersen RH, Hansen H, et al. Major intraoperative complications during video-assisted thoracoscopic anatomical lung resections: an intention-to-treat analysis. Eur J Cardiothorac Surg 2015;48:588-98; discussion 599. [Crossref] [PubMed]
- Byun CS, Lee S, Kim DJ, et al. Analysis of Unexpected Conversion to Thoracotomy During Thoracoscopic Lobectomy in Lung Cancer. Ann Thorac Surg 2015;100:968-73. [Crossref] [PubMed]
Cite this article as: Sawada S. A natural way to extend the indications for video-assisted thoracoscopic surgery in patients with advanced lung cancer. Video-assist Thorac Surg 2017;2:38.


