Does single-port video-assisted thoracic lobectomy have favorable perioperative results for non-small cell lung cancer compared with multi-port approach? A systematic review and meta-analysis
Introduction
Lung cancer was the first cause of cancer death among male and female worldwide (1). Surgical resection remains the mainstay therapy for patients with early stage non-small cell lung cancer (NSCLC). Soon after the first adoption of video-assisted thoracic surgery (VATS) lobectomy in early 1990s (2,3), growing evidence has demonstrated that VATS lobectomy is an alternative surgical approach for patients with early stage NSCLC, with regards to reduced postoperative pain, short length of hospital stay and even improved long-term survival when compared with open lobectomy (4-7). Even though, no standardized thoracoscopic technique has been established yet. Generally, most thoracic surgeons would like to take two, three or four ports VATS to perform lobectomy.
With the development of surgical techniques and instruments, single-port or uniportal VATS was introduced to the minimally invasive thoracic surgery gradually. Since the first report of single-port VATS lobectomy in 2011 (8,9), several studies have suggested that single-port VATS lobectomy is a safe and feasible surgical procedure for patients with lung cancer (10-13). Besides, some studies even showed that single-port VATS decreased postoperative pain and improved patients’ satisfaction when compared to conventional multi-port VATS (14,15). The preliminary clinical outcomes and short- and mid-term results of single-port VATS are encouraging (16,17). But whether single-port VATS lobectomy has favorable perioperative results for NSCLC compared with multi-port approach is still controversial. Thus, we take an attempt to perform the present systematic review and meta-analysis to evaluate the safety and perioperative efficacy of single-port VATS lobectomy for patients with NSCLC.
Methods
This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (18).
Search strategy
Published studies comparing single-port VATS to multi-port VATS lobectomy were identified by a comprehensive electronic search of PubMed, Embase, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and ClinicalTrials.gov up to December 2016. The search terms ‘single port’ OR ‘single incision’ OR ‘uniport’ OR ‘single access’ OR ‘single hole’ OR ‘one port’ OR ‘one incision’ AND ‘video-assisted thoracic surgery’ OR ‘VATS’ OR ‘thoracoscopic surgery’ were used to identify eligible comparative studies. In addition, we reviewed the reference lists of articles to identify further relevant citations.
Study selection
After removing the duplicates, the titles, abstracts and full-texts of references were evaluated by two reviewers (Shiyou Wei and Nan Chen) independently to find out the relevant studies. Studies were included if they were randomized controlled trials (RCT) or nonrandomized comparative studies comparing single-port VATS lobectomy to multi-port procedure for patients with NSCLC. Studies pertaining to single-port segmentectomy or wedge resection were excluded, since segmentectomy was technically more demanding than lobectomy. We also excluded studies that didn’t include a comparative group or didn’t provide at least one outcome of interest. Regarding duplicate data from the same center or hospital, we only included the latest and most updated article.
Data extraction and quality assessment
Two reviewers (Shiyou Wei and Nan Chen) independently assessed each included study and conducted data abstraction and quality assessment. Patients undergoing thoracoscopic lobectomy through a single incision were defined as single-port group and those who received thoracoscopic lobectomy performed by three or two incisions were defined as multi-port group. The outcome measures for this meta-analysis were operative time, perioperative blood loss, conversion rate, the number of lymph nodes dissection, postoperative pain, chest drainage duration, length of hospital stay, overall postoperative morbidity and mortality. The Newcastle-Ottawa Scale (NOS) was used to assess the risk of bias for each included observational study. Studies with scores more than 7 were considered to be high quality; conversely, those with scores lees than 3 were thought to be low quality. Any disagreements between the two reviewers were resolved be group discussion and the final determinations were performed by a senior reviewer (LLX).
Statistical analysis
Meta-analysis was performed by pooling the results of included studies. Pooled analysis for dichotomous variables such as overall postoperative morbidity, and conversion rate, was conducted by using the relative risks (RR) and their 95% confidence intervals (CI) with the Mantel-Haenszel method. And the standard mean differences (SMD) and their 95% CIs with Inverse-Variance method were calculated as the summary statistic for continuous variables such as operative time, perioperative blood loss and length of hospital stay. But if pooled analysis was impossible to perform as a result of heterogeneity in measurement methods among studies, descriptive analysis would be used to present the results of studies. And when studies reported results as median and range or interquartile range, these data were not included to conduct pooled analysis. All pooled outcome measures were determined by using random-effect models since the interventions varied among included studies. Statistical heterogeneity among the studies was assessed by means of a standard Cochrane’s Q test with a significance level of α=0.10. The I2 statistic test was performed to further examine clinical heterogeneity. I2≥50% was considered to indicate substantial heterogeneity. All P values were two-tailed, with P<0.05 suggesting statistical significant. All statistical analysis was carried out using Stata version 12.0 (StataCorp, College Station, TX, USA).
Results
Summary of included studies
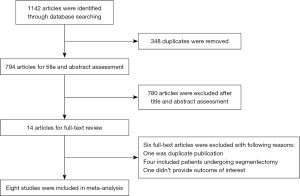
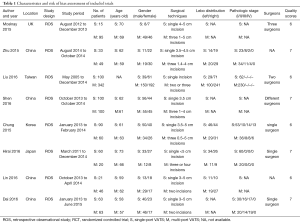
A flow chart summarizing the systematic literature selection is shown in Figure 1. A total of 1,142 publications (PubMed 934 publications, Embase 201 publications, Cochrane library three publications, and ClinicalTrials.gov four publications) were identified through the electronic searches and 348 of those were removing as a result of duplicates. After titles and abstracts review, 14 articles were selected for further evaluation. Finally, eight retrospective observational studies were included in this meta-analysis (19-26). A total of 1,257 patients were included in this meta-analysis, 482 (38.4%) in single-port group and 775 (61.6%) in multi-port group. Of these studies, seven studies were conducted in Asia and only one study in Europe. Two of these studies presented propensity-matched data. The quality of included studies assessed by the NOS was acceptable, with mean NOS scores of 6.5. For most studies, the methodological quality with regard to cohort selection and comparability was adequate. However, the follow-up periods were limited for all studies. The detailed characteristics and risk of bias assessment of included studies were shown in Table 1.
Full table
Assessment of perioperative outcomes
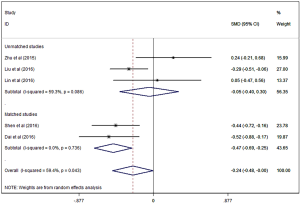
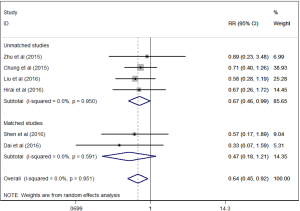
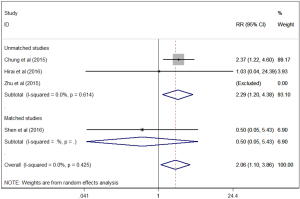
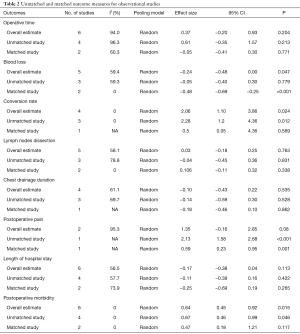
There was a statistically significant less perioperative blood loss for patients in single-port group compared to multi-port group (SMD =−0.24, 95% CI: −0.48 to 0, P=0.047, Figure 2). And single-port VATS lobectomy was significantly associated with lower overall postoperative morbidity rate than multi-port approach (RR=0.64, 95% CI: 0.45 to 0.92, P=0.015, Figure 3). But single-port approach was significantly associated with higher conversion rate than multi-port approach (RR =2.02, 95% CI: 1.10 to 3.73, P=0.024, Figure 4).
There were no statistically significant differences between single-port and multi-port VATS in regards to operative time (SMD =0.37, 95% CI: −0.20 to 0.93, P=0.204), the number of lymph nodes dissection (SMD =0.03, 95% CI: −0.18 to 0.25, P=0.763), postoperative pain (SMD =1.35, 95% CI: −0.16 to 2.85, P=0.08), chest drainage duration (SMD =−0.10, 95% CI: −0.43 to 0.22, P=0.535), and length of hospital stay (SMD =−0.17, 95% CI: −0.38 to −0.04, P=0.113). We failed to perform a pooled analysis on mortality between the two groups, since no deaths were reported in single-port group and only one death was shown in multi-port group (Table 2).
Full table
Assessment of propensity-matched data
When propensity-matched data were analyzed, there were no statistically significant differences between single-port and multi-port VATS in regards to overall morbidity, length of hospital stay, operative time, the number of lymph nodes dissection, conversion rate and chest drainage duration, but single-port approach was associated with less blood loss (SMD =-0.48; 95% CI: −0.69 to −0.25, P<0.001) and postoperative pain (SMD =−0.59, 95% CI: 0.23 to 0.95, P=0.001) when compared to multi-port approach (Table 2).
Discussion
The first description of single-port VATS took place in 1998 and concerned a series of six consecutive patients with pneumothorax (27). Later, Rocco and colleagues (28) reported their first experience of pulmonary wedge resection with single-port VATS in 2004. With the improvement of surgical techniques, Gonzalez-Rivas and colleagues reported complex single-port VATS lung resections including lobectomy (8), bronchial sleeve lobectomy (29), segmentectomy (30), pneumonectomy (31), and pulmonary vascular reconstruction and bronchoplasty (32) subsequently. And according to the latest reports (33,34), single-port VATS can be applied to lobectomy and wedge resection in non-intubated patients. Indeed, it is a challenging technique for most thoracic surgeons, since three or four thoracoscopic items were placed through a single incision at the same time, which may restrict surgeons’ maneuvering (10,35). However, advocates of single-port VATS emphasize that this approach has close resemblance to open approach in terms of dissecting, isolating, and dividing hilar structures, which provides a direct view for surgeons to target structures (10,12,16).
To our knowledge, this is the first systematic review and meta-analysis comparing single-port VATS to multi-port VATS lobectomy for patients with NSCLC. This meta-analysis indicated that single-port VATS lobectomy was associated with less blood loss and lower overall postoperative morbidity, but higher conversion rate than multi-port approach. However, these findings should be interpreted with caution, as high selection of patients at the beginning of a new surgical technique should be taken into consideration. Moreover, when propensity-matched data were analyzed, single-port approach was associated with less blood loss and postoperative pain. Overall, these findings suggested that single-port VATS lobectomy is a safe and feasible procedure for NSCLC in selected cases, but there has been insufficient evidence to prove its superior short-term effects than multi-port approach so far.
Single-port VATS lobectomy was associated with higher conversion rate among unmatched studies in this meta-analysis, but there was no significant difference among matched studies. Chung and colleagues (23) reported a conversion rate as high as 35.5% in patients undergoing single-port VATS lobectomy, but Shen and colleagues (22) just reported one conversion to two-port VATS lobectomy and another conversion to open thoracotomy; and Hirai and colleagues (24) also showed only one conversion to open lobectomy. This can be explained in part by the learning curve that is associated with a new surgical approach. With the improvement of surgeons’ experience and surgical technique, the conversion rate single-port VATS lobectomy can be comparable to multi-port approach. On the other hand, Chung and colleagues (23) noted the reasons for conversion. In their study, most conversions were two-port VATS mainly due to diffuse, tight pleural adhesions and hilar lymph nodes, and the main reasons for conversion to three-port VATS or open lobectomies were due to tumor location and bronchial injury occurred in the initial single-port approach. And this indicated that single-port VATS lobectomy may be still difficult to deal with highly complex cases when compared with multi-port approach.
Previous studies have showed that when compared with multi-port VATS, single-port approach was associated with less postoperative pain in patients with pneumothorax (36-38). This superiority may benefit from the reduction in the number of intercostal spaces and avoiding the use of a trocar in the procedure, which minimized the risk of intercostal nerve injury (16). That is to say, less postoperative pain may be a potential advantage for single-port VATS when compared to multi-port approach. In our meta-analysis, decreased postoperative pain in single-port VATS lobectomy was observed among matched studies, but there was no significant difference among unmatched studies. Since pain was assessed at various time points with different scales in most included studies, only two studies with same time points and scales were included for meta-analysis and there was significant heterogeneity between the two studies. Thus, this finding should be interpreted with caution, and further studies with standardized pain management protocols are necessary.
There are several limitations existing in this systematic review and meta-analysis. Firstly, only eight retrospective studies were included to conduct this meta-analysis. Considering the quantity and quality of included studies, our results should be interpreted with caution. Secondly, specific criteria for the definition of outcomes, such as conversion and morbidity, were not clearly stated in most included studies. Thirdly, we failed to pool the analysis of outcomes in terms of quality of life, cost-effectiveness, and long-term survival outcomes of single-port VATS versus multi-port VATS lobectomy.
In summary, single-port VATS lobectomy is a safe and feasible procedure for patients with NSCLC in selected cases, but there has been insufficient evidence to prove its superior short-term effects than multi-port approach so far. And further well designed studies with long-term follow-up outcomes are necessary to assess each advantages and indications for single-port and multi-port VATS lobectomy.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2017.05.04). Liu L serves as the Editor-in-Chief of Video-Assisted Thoracic Surgery. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA: a cancer journal for clinicians 2015;65:87-108. [Crossref] [PubMed]
- Walker WS, Carnochan FM, Pugh GC. Thoracoscopic pulmonary lobectomy. Early operative experience and preliminary clinical results. J Thorac Cardiovasc Surg 1993;106:1111-7. [PubMed]
- Kirby TJ, Mack MJ, Landreneau RJ, et al. Initial experience with video-assisted thoracoscopic lobectomy. Ann Thorac Surg 1993;56:1248-52; discussion 52-3. [Crossref] [PubMed]
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [Crossref] [PubMed]
- Cao C, Manganas C, Ang SC, et al. A meta-analysis of unmatched and matched patients comparing video-assisted thoracoscopic lobectomy and conventional open lobectomy. Ann Cardiothorac Surg 2012;1:16-23. [PubMed]
- Chen FF, Zhang D, Wang YL, et al. Video-assisted thoracoscopic surgery lobectomy versus open lobectomy in patients with clinical stage non-small cell lung cancer: a meta-analysis. Eur J Surg Oncol 2013;39:957-63. [Crossref] [PubMed]
- Taioli E, Lee DS, Lesser M, et al. Long-term survival in video-assisted thoracoscopic lobectomy vs open lobectomy in lung-cancer patients: a meta-analysis. Eur J Cardiothorac Surg 2013;44:591-7. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:539-41. [Crossref] [PubMed]
- Tam JK, Lim KS. Total muscle-sparing uniportal video-assisted thoracoscopic surgery lobectomy. Ann Thorac Surg 2013;96:1982-6. [Crossref] [PubMed]
- Feng M, Shen Y, Wang H, et al. Uniportal video assisted thoracoscopic lobectomy: primary experience from an Eastern center. J Thorac Dis 2014;6:1751-6. [PubMed]
- Ibrahim M, Menna C, Andreetti C, et al. Flexible videoscope for thoracoscopic lobectomy: evolution of uniportal technique. Surg Endosc 2015;29:2056-9. [Crossref] [PubMed]
- Kim HK, Choi YH. The feasibility of single-incision video-assisted thoracoscopic major pulmonary resection performed by surgeons experienced with a two-incision technique. Interact Cardiovasc Thorac Surg 2015;20:310-5. [Crossref] [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [Crossref] [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Ng CS, Kim HK, Wong RH, et al. Single-Port Video-Assisted Thoracoscopic Major Lung Resections: Experience with 150 Consecutive Cases. Thorac Cardiovasc Surg 2016;64:348-53. [Crossref] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [Crossref] [PubMed]
- McElnay PJ, Molyneux M, Krishnadas R, et al. Pain and recovery are comparable after either uniportal or multiport video-assisted thoracoscopic lobectomy: an observation study. Eur J Cardiothorac Surg 2015;47:912-5. [Crossref] [PubMed]
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [PubMed]
- Liu CC, Shih CS, Pennarun N, et al. Transition from a multiport technique to a single-port technique for lung cancer surgery: is lymph node dissection inferior using the single-port technique?†. Eur J Cardiothorac Surg 2016;49:i64-72. [PubMed]
- Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study†. Eur J Cardiothorac Surg 2016;49:i48-53. [PubMed]
- Chung JH, Choi YS, Cho JH, et al. Uniportal video-assisted thoracoscopic lobectomy: an alternative to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015;20:813-9. [Crossref] [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomesdagger. Eur J Cardiothorac Surg 2016;49:i37-41. [Crossref]
- Dai F, Meng S, Mei L, et al. Single-port video-assisted thoracic surgery in the treatment of non-small cell lung cancer: a propensity-matched comparative analysis. J Thorac Dis 2016;8:2872-8. [Crossref] [PubMed]
- Lin F, Zhang C, Zhang Q, et al. Uniportal video-assisted thoracoscopic lobectomy: An alternative surgical method for pulmonary carcinoma. Pak J Med Sci 2016;32:1283-5. [PubMed]
- Yamamoto H, Okada M, Takada M, et al. Video-assisted thoracic surgery through a single skin incision. Arch Surg 1998;133:145-7. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. [Crossref] [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Video: Single-incision video-assisted thoracoscopic right pneumonectomy. Surg Endosc 2012;26:2078-9. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, de la Torre M, et al. Bronchovascular right upper lobe reconstruction by uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2014;6:861-3. [PubMed]
- Hung MH, Cheng YJ, Chan KC, et al. Nonintubated uniportal thoracoscopic surgery for peripheral lung nodules. Ann Thorac Surg 2014;98:1998-2003. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014;19:552-5. [Crossref] [PubMed]
- Zhu Y, Xu G, Zheng B, et al. Single-port video-assisted thoracoscopic surgery lung resection: experiences in Fujian Medical University Union Hospital. J Thorac Dis 2015;7:1241-51. [PubMed]
- Kang do K. Early outcomes of single-port video-assisted thoracic surgery for primary spontaneous pneumothorax. Korean J Thorac Cardiovasc Surg 2014;47:384-8. [Crossref] [PubMed]
- Song IH, Lee SY, Lee SJ. Can single-incision thoracoscopic surgery using a wound protector be used as a first-line approach for the surgical treatment of primary spontaneous pneumothorax? A comparison with three-port video-assisted thoracoscopic surgery. Gen Thorac Cardiovasc Surg 2015;63:284-9. [Crossref] [PubMed]
- Chen PR, Chen CK, Lin YS, et al. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax. J Cardiothorac Surg 2011;6:58. [Crossref] [PubMed]
Cite this article as: Wei S, Chen N, Liu C, Zhao K, Zhu L, Liu L. Does single-port video-assisted thoracic lobectomy have favorable perioperative results for non-small cell lung cancer compared with multi-port approach? A systematic review and meta-analysis. Video-assist Thorac Surg 2017;2:33.