A case of Mullerian cyst resected by video assisted thoracoscopic surgery
Introduction
Posterior mediastinum is common location of neurogenic tumours and neurenteric cysts. In 2005, Hattori described so far unknown cyst of this region, with probable Mullerian histogenesis (1).
We report a case of 53-year-old woman with Mullerian congenital cyst that was resected using video-assisted thoracic surgery (VATS) approach.
Case presentation
A 53-year-old, non-smoking woman was admitted to thoracic surgery clinic for suspicion of neuroma of posterior mediastinum. Tumour was accidentally detected in chest radiograph. After initial diagnostics in pulmonary clinic patient was qualified for surgery. Patient did not report any symptoms. Patient was taking hormone replacement therapy.
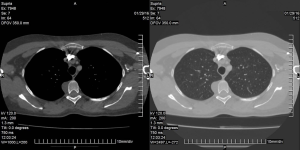
Physical examination and laboratory tests did not presented any abnormalities. The chest computed tomography (CT) demonstrated a cystic mass in right lateral part of the 4th vertebra, 22 mm × 30 mm × 15 mm in size (Figure 1). Magnetic resonance imaging of the chest was not performed. In radiological imaging neurenteric cyst was diagnosed. The mass was removed using VATS two-portal approach (4th anterior axillary and 6th middle axillary intercostals space). Camera revealed lucent cyst with thin wall. During operation the cyst was opened and yellow fluid was evacuated. Rest of tissues was dissected and removed. Location of resected mass was coagulated using argon plasma coagulation. Chest drain was removed in second day after operation.
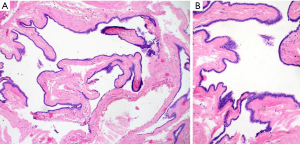
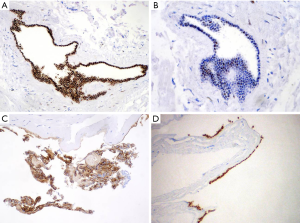
In the microscopic examination there were pieces of fibrous connective tissue with a single smooth muscle fiber. In the center there was cystic lesion lined by single layer of cuboidal epithelial cells without papillary structures or mucin secretion. Epithelium did not demonstrate cellular atypia and there were no mitosis. Differential diagnosis taken under consideration was Mullerian cyst, enteric cyst and unusual variant of bronchogenic cyst. Additional immunohistochemistry (IHC) tests had been processed. Pan-Cytokeratins (CK AE1/AE3), cytokeratin 7 (CK7) and estrogen receptor (ER) were homogeneously, strongly positive. Focal expression of transcription factor PAX8, progesterone receptor (PR) and cancer antigen 125 (CA125) were noticed. A few epithelial cells were also stained by anty-CD56 antibody. Staining for thyroid transcription factor (TTF-1), cytokeratin 20 (CK20), CDX2 were uniformly negative. Ki-67 mitotic index were less than 1%. The final diagnosis was Mullerian cyst (Hattori’s cyst) due the microscopic image and typical ER, PR, Ca125 and PAX8 staining (Figures 2,3).
Patient’s postoperative course was uneventful. She was discharged on the third after surgery.
Discussion
Mullerian cysts are typically observed in genitourinary organs in pelvic region (2). Since first report in 2005 by Hattori two retrospective studies concerning mentioned cysts were performed. Hattori found this mass in 3 of 19 cases of mediastinal cysts (15.8%). However, in larger patient group Thomas-de-Montarville confirmed only 7 cases of Mullerian cyst from 163 mediastinal cysts (4.3%) (2,3). In our clinical experience it was first incidence of these pathology.
The histogenesis of Mullerian cyst in the mediastinum is unknown. According to Ludwig’s theory—lesion is a result of agenesis of primary Mullerian apparatus. In Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome similar pathogenesis is observed (2,4). However, Hattori affirm that the cysts are misplaced mesothelium with Mullerian characteristics.
According to Kabayashi’s study—Mullerian cysts usually occur in woman at the age of 40 to 60. Only Hattori in his original study reported this cyst in 18-year-old patient (2,4). Typical location of pathology is paravertebral space between 3rd and 8th thoracic vertebra (3,4). Our patient was a 53-year-old woman and cyst was located in paravertebral region of 4th vertebra. The most common symptoms are cough and chest pain. Dakak et al. reported a patient with dysphagia (5). Our patient did not notice any symptoms. Most Mullerian cysts of mediastinum occur in pre menopausal period. Obesity, hormone replacement therapy, a hysterectomy and an oophorectomy is also observed in many cases. Our patient was in menopausal period and was using hormonal replacement therapy. Differential diagnosis includes neurenteric, bronchogenic, gastroenteric and mesothelial and thoracic duct cysts. In microscope imaging typical neurogenic cysts are lined by columnar cells with neural or enteric differentiation, while mesothelial cysts are lined by a single mesothelial cells layer. Thoracic duct cyst may not communicate with the duct and is lined by respiratory or squamous epithelium. Enterogenous and bronchogenic cysts have lined by columnar epithelium with a smooth muscle bundles as well as Mullerian cyst (5). IHC confirm negative expression or weakly positive of cytokeratin 5/6, and positive expression of ER and PR. ER and PR are considered to be the best markers of Mullerian cysts. In presence case ER was positive and PR focally positive. Recurrences were not reported.
In conclusion female patient in between 40 to 60 years of age with obesity or gynecological history and with cyst in paravertebral location is considered to differential diagnosis for Mullerian cyst.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2017.05.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hattori H. High prevalence of estrogen and progesterone receptor expression in mediastinal cysts situated in the posterior mediastinum. Chest 2005;128:3388-90. [Crossref] [PubMed]
- Kobayashi S, Inoue T, Karube Y, et al. A case of Mullerian cyst arising in posterior mediastinum. Ann Thorac Cardiovasc Surg 2012;18:39-41. [Crossref] [PubMed]
- Chon SH, Im UJ, Song DS. Paravertebral mediastinal Mullerian cyst resected by video assisted thoracoscopic surgery. J Thorac Dis 2015;7:E47-9. [PubMed]
- Simmons M, Duckworth LV, Scherer K, et al. Mullerian cysts of the posterior mediastinum: report of two cases and review of the literature. J Thorac Dis 2013;5:E8-10. [PubMed]
- Dakak M, Poyraz B, Bulut S, et al. An unusual cyst of posteriori mediastinum: Mullerian cyst. Turk Gogus Kalp Dama 2015;23:154-6. [Crossref]
Cite this article as: Łochowski M, Kuncman W, Rębowski M, Kozak J. A case of Mullerian cyst resected by video assisted thoracoscopic surgery. Video-assist Thorac Surg 2017;2:31.