
Uniportal video-assisted thoracic surgery in the diagnosis of mediastinal lymphadenopathy of unknown aetiology
Introduction
Patients with mediastinal lymphadenopathy require an accurate diagnosis to determine as soon as possible an optimal treatment. During the past decade, real-time endobronchial ultrasound guided transbronchial needle aspiration (EBUS-TBNA) has become a safe technique for staging lung cancer (1-3).
EBUS-TBNA combines endoscopic visualisation with high-frequency ultrasound imaging, which is used to obtain tissue samples of mediastinal lesions adjacent to the tracheobronchial tree, under sedation in the outpatient setting (4). As many authors reported, EBUS-TBNA had a sensitivity of more than 90% (5,6) equivalent to or even superior to that of mediastinoscopy and had lower associated costs and fewer morbidities (7). Now EBUS-TBNA is the first line procedure for the diagnosis of benign and malignant lesions of the mediastinum (lymphoma, lung cancer, sarcoidosis, tuberculosis, etc.).
However, also EBUS-TBNA has its limitations, either because some areas in the mediastinum are inaccessible for this procedure or because of its false negative rate. The main aim of our study was to evaluate the reliability of video-assisted thoracic surgery (VATS) in obtaining a histological diagnosis of mediastinal lymph nodes (in all areas of mediastinum) and define its role in subsequent workup and treatment plan for these patients.
Methods
We retrospectively reviewed 136 patients who underwent to VATS biopsy of mediastinal lymphadenopathy from January 2003 to December 2013 at the Department of Thoracic Surgery of AUSL Romagna, and data were retrieved from individual medical records. Patients with mediastinal lymphadenopathy of unknown aetiology (also those with a previous history of lung cancer or others extrapulmonary malignancy) were identified and were considered eligible for VATS biopsy by traditional staging with chest radiography, bronchoscopy, thoracic/abdominal/brain CT. All 136 patients were investigated by CT scan, performed not later than 30 days from the surgery, and 92 patients were also evaluated by positron emission tomography (PET)/CT with fluorodeoxyglucose.
The lymph node stations of the mediastinum and hilar regions were designated according to the International Staging System (8).
Surgical technique
All patients were operated on under general anaesthesia with double-lumen endotracheal intubation. All were positioned in the lateral decubitus, and in all cases, only one incision (2–2.5 cm) is placed in the fifth intercostal space along the middle axillary line (9-11). Sometimes, for high lymph node stations as left 5–6 lymph node stations or 2–4 stations, the incision is placed in the fourth or third intercostal place along the middle axillary line. A 30° 5-mm video thoracoscope and 5-mm endoscopic instruments were used. The targeted nodal station is approached, and the mediastinal pleura is opened by endoscissors or terminal devices. The nodes are sampled with a biopsy forceps, in a fashion similar to the traditional mediastinoscopy procedure. If it is possible, the entire lymph node is excised, and an endoclip is fired at the base of the vascular pedicle. Adequate haemostasis is obtained with use of endoclips, coagulation, thermal devices. We used a singular 28 French thoracic tube to drain the mediastinum for 1–2 days. The uniportal-VATS biopsies were uneventful, and there were no complications for the patients.
Statistical analysis
Patient characteristics are reported as means ± standard deviations or n (%), as appropriate. Overall survival (OS) was defined as the time from date of surgery to death due to any cause.
Results
One hundred thirty-six patients were identified from our database (85 men, and 51 women), mean age 57±17 and underwent to VATS surgery and no complications were observed. The final diagnosis was obtained by final pathologic confirmation in all the patients.
All 136 patients underwent to definitive VATS biopsy, in all of these areas of mediastinum with a sensitivity and a specificity of 100%.
A malignant mediastinal process was diagnosed in 114 patients and a benign process in 21 patients.
Malignant lymphoma was the most frequently seen malignant mediastinal tumour (n=43) (Table 1). There were 25 cases of lung cancer, 28 cases of thymoma, 16 cases of lymph node metastases from epithelial tumours of extrathoracic origin, 2 cases of sarcoma.
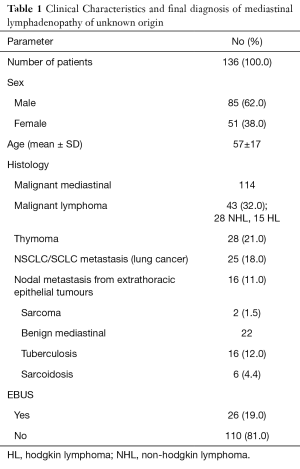
Full table
The benign mediastinal lymphadenopathies consisted of sarcoidosis (n=6), and tuberculosis (n=16).
The pretracheal and subcarinal lymph node stations (3a-7) were the site of biopsy in 34 (25%) patients, paratracheal lymph node (R2–4/L2–4) were the site of biopsy in 16 (12%) patients. Para-aortic and subaortic nodes [5–6] were the site of biopsy in 35 (26%) patients, para-esophageal and pulmonary ligament nodes (R-L8–9) were the site of biopsy in 23 (17%) patients. Twenty-seven (20%) patients had only hilar lymph nodes (R-L10) sampled (Table 2).
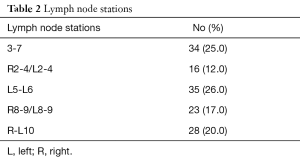
Full table
After a mean follow-up of 38 months, 65 (45%) patients are alive. Twenty-six (19%) patients had previous negative EBUS-TBNA with a VATS diagnosis of malignant disease in 15 cases. Mean hospital stay was 2±1.8 days.
Discussion
EBUS-TBNA is an accurate and safe tool in the diagnosis of benign and malign mediastinal lymphadenopathies. It can necessarily be the first-line procedure in these patients, but it cannot completely replace surgery.
EBUS-TBNA requires considerable training to acquire adequate competence [previously significant improvement in diagnostic performance was seen after the completion of 20 procedures and diagnostic accuracy did not peak until after 50 procedures (11)].
Besides, there is controversy regarding the role of small volume diagnostic specimens for the diagnosis of lymphoma, and cytological diagnosis of lymphoma is harder than that for epithelial tumours. For these reasons, today many authors prefer surgical biopsy for patients with suspicious of mediastinal lymphoma.
Thoracoscopic approach to a mediastinal lymphadenopathy requires a significant experience in VATS but is a safe and accurate procedure for these patients (12). It can necessarily be a second-line procedure for the majority of cases. Also, it can be essential for those patients with negative EBUS-TBNA but with high suspicion of mediastinal disease (EBUS false-negative) and for those with lymphadenopathies in not accessible areas of the mediastinum. Indeed, EBUS-TBNA has the inability to access some parts of the mediastinum and in particular the anterior and posterior mediastinum. The posterior mediastinum may be accessible by EUS-FNA, and some authors believe that by combining EBUS-TBNA and EUS-FNA the majority of the mediastinum is accessible (13,14). However, even with this combination, the anterior mediastinum is tough to access; in our experience stations, L5–6 are not manageable with this EBUS-TBNA.
VATS is feasible for all areas of the mediastinum, with a sensitivity of 100% and a specificity and overall accuracy of 100%. In our population of 26 (19%) cases of EBUS-TBNA negative, VATS permitted to obtain a particular diagnosis of disease (11 cases of benign disease and 15 cases of malignant lymphadenopathies).
In the competent hands, VATS is an accurate and safe procedure in the diagnosis of mediastinal and hilar lymphadenopathy, and sometimes, it can necessarily be the first-line procedure. Also, it requires considerable training to acquire competence in different areas of the mediastinum, especially with uniportal technique. However, it should always be considered for evaluation of mediastinal lymphadenopathies in non-accessible areas and in all cases in which TBNA failed to obtain a diagnosis, but it is highly suspicious of disease. In our experience is crucial to offer patients with the mediastinal disease a multidisciplinary approach in which different experiences (pneumologist, surgeon, endoscopist) may compare and identify the best diagnostic procedure for the patient.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2018.09.04). LB serves as an unpaid editorial board member of Video-Assisted Thoracic Surgery from Jul 2016 to May 2019. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was given by all patients. IRB for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Varela-Lema L, Fernández-Villar A, Ruano-Ravina A. Effectiveness and safety of endobronchial ultrasound-transbronchial needle aspiration: a systematic review. Eur Respir J 2009;33:1156-64. [Crossref] [PubMed]
- Trisolini R, Lazzari Agli L, Patelli M. Conventional vs endobronchial ultrasound-guided transbronchial needle aspiration of the mediastinum. Chest 2004;126:1005-6. [Crossref] [PubMed]
- Herth FJ, Eberhardt R, Vilmann P, et al. Real-time endobronchial ultrasound guided transbronchial needle aspiration for sampling mediastinal lymph nodes. Thorax 2006;61:795-8. [Crossref] [PubMed]
- Yasufuku K, Chiyo M, Koh E, et al. Endobronchial ultrasound guided transbronchial needle aspiration for staging of lung cancer. Lung Cancer 2005;50:347-54. [Crossref] [PubMed]
- Medford AR, Bennett JA, Free CM, et al. Mediastinal staging procedures in lung cancer: EBUS, TBNA and mediastinoscopy. Curr Opin Pulm Med 2009;15:334-42. [Crossref] [PubMed]
- Yasufuku K, Chiyo M, Sekine Y, et al. Real-time endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest 2004;126:122-8. [Crossref] [PubMed]
- Lemaire A, Nikolic I, Petersen T, et al. Nine-year single center experience with cervical mediastinoscopy: complications and false negative rate. Ann Thorac Surg 2006;82:1185-9; discussion 1189-90. [Crossref] [PubMed]
- Mountain CF, Dresler CM. Regional lymph node classification for lung cancer staging. Chest 1997;111:1718-23. [Crossref] [PubMed]
- Solaini L, Prusciano F, Bagioni P, et al. Video-assisted thoracic surgery major pulmonary resections. Present experience. Eur J Cardiothorac Surg 2001;20:437-42. [Crossref] [PubMed]
- Solaini L, Prusciano F, Bagioni P, et al. Video-assisted thoracic surgery (VATS) of the lung: analysis of intraoperative and postoperative complications over 15 years and review of the literature. Surg Endosc 2008;22:298-310. [Crossref] [PubMed]
- Rocco G, Brunelli A, Jutley R, et al. Uniportal VATS for mediastinal nodal diagnosis and staging. Interact Cardiovasc Thorac Surg 2006;5:430-2. [Crossref] [PubMed]
- Steinfort DP, Hew MJ, Irving LB. Bronchoscopic evaluation of the mediastinum using endobronchial ultrasound: a description of the first 216 cases carried out at an Australian tertiary hospital. Intern Med J 2011;41:815-24. [Crossref] [PubMed]
- Solaini L, Bagioni P, Campanini A, et al. Diagnostic role of videothoracoscopy in mediastinal diseases. Eur J Cardiothorac Surg 1998;13:491-3. [Crossref] [PubMed]
- Vilmann P, Krasnik M, Larsen SS, et al. Transesophageal endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) biopsy: a combined approach in the evaluation of mediastinal lesions. Endoscopy 2005;37:833-9. [Crossref] [PubMed]
Cite this article as: Lo Faso F, Bertolaccini L, Davoli F, Bagioni P, Zago S, Solli P. Uniportal video-assisted thoracic surgery in the diagnosis of mediastinal lymphadenopathy of unknown aetiology. Video-assist Thorac Surg 2017;2:27.


