Our novel procedure for thoracoscopic anatomical segmentectomy
Introduction
Currently, anatomic lobectomy is the standard treatment for all operable non-small cell lung cancers (NSCLCs), while sublobar resections have traditionally been used as parenchymal sparing procedures in patients with significantly reduced pulmonary function. In recent years, adenocarcinoma has been given two new unique classifications: adenocarcinoma-in-situ and minimally invasive adenocarcinoma (1). As they are rarely considered to be associated with nodal involvement, many studies of intentional limited resection have investigated these adenocarcinomas, which are either pure ground-glass nodule (GGN) or part solid GGN on computed tomography (CT). Excellent surgical outcomes, with no evidence of recurrence after sublobar resection, have been demonstrated (2).
It is reasonable to perform a less invasive resection of a smaller volume of the lung tissue. This simple procedure of wedge resection may be sufficient if the tumors were located in the peripheral sub-pleural parenchyma. However, wedge resection is inadequate for a lesion located deep in the lung. Segmentectomy is preferred in such cases to secure an adequate surgical margin (3). In open thoracotomy surgery, a tumor is dissected bluntly by maintaining a sufficient margin while directly palpating the tumor. However, in a thoracoscopic surgery in which the surgeon`s hand cannot be passed directly into the thoracic cavity, it is important to have a clear anatomical understanding before proceeding with the operation.
Patient selection and work up
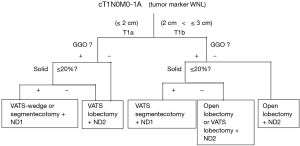
Our basic selection criteria for thoracoscopic segmentectomy were as follows: (I) a tumor size less than 2 cm, and a solid component ratio less than 20%, If the tumors is considered to be a lung cancer. Moreover, the selection of procedures between wedge resection and segmentectomy depend on the tumor location and the GGO ratio (Figure 1); (II) patients with compromised resection compromised patients who were considered to be poor candidates for lobectomy because of limited cardiopulmonary reserve or other comorbidities (III) patients with metastases, and (IV) patients with benign lesions.
Wedge resection was considered to be inappropriate in all cases because of the tumor size or location in the deep parenchyma. Written informed consent was obtained from all patients.
Standard blood, spirometric tests and electrocardiography for patients undergoing thoracic operation are mandatory. The other requirements for surgery is a reliable confirmation of a CT scan of the chest.
Preoperative preparation
Preoperative CT simulation is important. With rapid advances in multi-detector CT (MDCT) in recent years, it has become possible to easily perform three-dimensional (3D) processing not only in a workstation but also on an operating room.
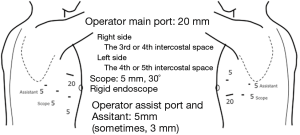
By using MDCT, we understand each patient’s individual anatomy and can perform operations mainly by defining the course of arteries and veins. Usually in many hospitals, radiologists or technicians construct the 3D image using a workstation. The arteries and the veins are separately segmented and color-coded by CT value, and these volume-rendered images are then merged into the 3D-CT angiography. This image is ideal but it takes a long time to create. Thoracic surgeons know the basic anatomy of the lung, and therefore don’t need complex images. When we use volume rendering methods, we prepare simple images that meet our needs in as little time as approximately seven minutes and by cutting out the area of interest, the image can be magnified, de-magnified or rotated during surgery (Figure 2) (4). We previously reported that port-access thoracoscopic segmentectomy could be safely be performed in all segments using this approach, termed Segmentectomy Achieved by MDCT for Use in Respective Anatomical Interpretation (SAMURAI) (5).
Equipment preference card
No special instrument is needed. The HARMONIC or ENSEAL or LIGASURE device make it easier to dissection of segmental vessels and lung parenchyma.
Procedure
We collapsed the lung on the operating side to anesthetize the patients under differential ventilation. During the procedure, the surgeons stood on the ventral side of the patient and the assistants stood on the dorsal side. The image, on the side of the assistants, was rotated 180 degrees. Four ports (one with a diameter of 20 mm, and three with a diameter of 5 mm) were prepared for the port-access technique (6) (Figure 3).
Previously, we first treated the segmental artery and bronchus at the pulmonary hilum and then the pulmonary parenchyma was incised. However, it was not possible to cover resection of all segments with this method alone.
As the segmental artery is located at the pulmonary hilum in the superior segment of the lower lobe, identification and dissection are relatively easy. However, as arterial branches are embedded in the pulmonary parenchyma in some segments, it is sometimes necessary to preserve the proximal branch and divide the peripheral branch.
The venous branches within the segment become intersegmental veins as they concentrate, and return to the hilum. In segmentectomy, it is very important to understand these intersegmental and intra-segmental veins.
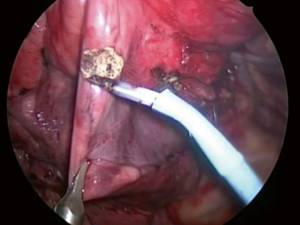
In recent cases, we first dissected the pulmonary parenchyma along the intersegmental vein using an energy device or an electrical cautery, and the intrasegmental vein was identified (Figure 4) (7). The division of the intrasegmental veins allows for the identification of the intersegmental border and facilitates further parenchymal dissection. Subsequently, we could reach the target artery and bronchus (8).

The basis of segmentectomy is to isolate and divide the bronchus and then dissect its peripheral pulmonary parenchyma. For conventional segmentectomy in open thoracotomy, division at the intersegmental border has been generally performed by dissecting the bronchus in the target lung and collapsing the lung on the peripheral side.
In this situation, jet ventilation has been reported useful as an inflation method for the affected segment in thoracoscopic surgery or small thoracotomy (9). However, this method requires equipment and another doctor to maneuver the bronchoscope. Some institutions experienced such difficulties and various modifications have been devised. Direct inflation into the bronchus using a buttery needle from the operative field was reported to be useful (10). However, great care is warranted as this approach can reportedly cause an air embolism.
Moreover, we experienced that some young unskillful anesthetist could not insert the bronchoscope into the smaller bronchi. Therefore, we attempted to block the bronchus by ligation with expansion of the affected segment. We ligated a bronchus conventionally using a knot pusher after ventilation when the bronchus was narrow.
We found the slip-knot technique using 3-0 or 4-0 monofilament thread customized from the previously reported modified Roeder knot was useful since it enabled the surgeon to ligate the bronchus during ventilation of the lung. The bronchus is then closed by pulling the thread (Figures 5,6) (11), and is effective for creating an inflation-deflation line (Figure 7) (12). We believe that this method can be generalized because it does not require any special equipment and is applicable at any time.

We dissected the parenchyma along the inflation-deflation line, using an energy device or electrical cautery at the hilum as well as staplers. In lung cancer surgery, the surgical margin is more important than the inflation-deflation line, therefore, sometimes we perform a larger dissection of the lung parenchyma.
Conclusions
Anatomical thoracoscopic segmentectomy is seems to be one of the most complicated surgery. But, comprehension of the intersegmental and intrasegmental veins using 3DCT simulation and creation of an inflation-deflation line by using a method of inflating the affected segment can be performed safely adequate surgical margin.
Role of team members
To manage effectively patients undergoing segmentectomy there must be a well organized team consisting of several specialists, operative treatment and postoperative care of patients.
- Thoracic surgeons—selection of patients for segmentectomy, performance of an operation in minimally invasive technique.
- Anaesthesiologists—proper conducting of anaesthesia.
- Nurses—care of patients before and after an operation.
Tips, tricks and pitfalls
We consists several knacks and tips in order to perform successful thoracoscopic segmentectomy.
One is using 3D image by computed tomography angiography, which enables precise understanding the complicated individual anatomy of pulmonary vessels. Second is an effective use of energy devices and staplers. We uses energy device to divide intersegmental plane in the center of lung, referring intersegmental veins. On the other hand, stapler is used in the peripheral lung.
Third is a slipknot on the resecting small bronchus, which closes the resecting bronchus in a moment, while using inflation- deflation method to show intersegmental line.
Above all, the importance of safe surgery due to precise and spatial understanding of anatomy cannot be overemphasized. And as a cancer surgery, no inferior survival outcome is necessary, as well as better postoperative QOL and less morbidity.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2017.04.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2011;6:244-85. [Crossref] [PubMed]
- Schuchert MJ, Pettiford BL, Keeley S, et al. Anatomic segmentectomy in the treatment of stage I non-small cell lung cancer. Ann Thorac Surg 2007;84:926-32; discussion 932-3. [Crossref] [PubMed]
- Koike T, Kitahara A, Sato S, et al. Lobectomy Versus Segmentectomy in Radiologically Pure Solid Small-Sized Non-Small Cell Lung Cancer. Ann Thorac Surg 2016;101:1354-60. [Crossref] [PubMed]
- Suzuki J, Oizumi H, Kato H, et al. Surgeon makes Three-dimensional computed tomography angiography in operating room. Asvide 2017;4:177. Available online: http://www.asvide.com/articles/1485
- Oizumi H, Endoh M, Takeda S, et al. Anatomical lung segmentectomy simulated by computed tomographic angiography. Ann Thorac Surg 2010;90:1382-3. [Crossref] [PubMed]
- Oizumi H, Kanauchi N, Kato H, et al. Anatomic thoracoscopic pulmonary segmentectomy under 3-dimensional multidetector computed tomography simulation: a report of 52 consecutive cases. J Thorac Cardiovasc Surg 2011;141:678-82. [Crossref] [PubMed]
- Suzuki J, Oizumi H, Kato H, et al. Dissecting the pulmonary parenchyma (between S1 and S3) along the intersegmental vein (V1b) using an energy device in S1 segmentectomy. Asvide 2017;4:178. Available online: http://www.asvide.com/articles/1486
- Oizumi H, Kato H, Endoh M, et al. Techniques to define segmental anatomy during segmentectomy. Ann Cardiothorac Surg 2014;3:170-5. [PubMed]
- Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg 2007;133:753-8. [Crossref] [PubMed]
- Kamiyoshihara M, Kakegawa S, Ibe T, et al. Butterfly-needle video-assisted thoracoscopic segmentectomy: a retrospective review and technique in detail. Innovations (Phila) 2009;4:326-30. [Crossref] [PubMed]
- Suzuki J, Oizumi H, Kato H, et al. Slip knot technique video. Asvide 2017;4:179. Available online: http://www.asvide.com/articles/1487
- Oizumi H, Kato H, Endoh M, et al. Slip knot bronchial ligation method for thoracoscopic lung segmentectomy. Ann Thorac Surg 2014;97:1456-8. [Crossref] [PubMed]
Cite this article as: Suzuki J, Oizumi H, Kato H, Endoh M, Hamada A, Watarai H, Nakahashi K, Sadahiro M. Our novel procedure for thoracoscopic anatomical segmentectomy. Video-assist Thorac Surg 2017;2:26.