
A novel approach for minimally invasive everted esophagectomy in pigs
Introduction
Esophagectomy generally incorporates procedures from two or three different surgical fields (1,2), resulting in substantial surgical damage. Minimally invasive esophagectomy (MIE) is a good approach that can reduce the surgical injury compared with open surgery methods (3). But no surgeon would give up the efforts to improve surgical procedures. In this paper, we designed a novel operative procedure, minimally invasive everted esophagectomy in pigs.
Methods
Animals
For the purposes of this study, three pigs (Sus domesticus) were provided by Johnson & Johnson China Ltd. The experiment was conducted in the Beijing science center of Johnson & Johnson China Ltd. The studies were approved by Animal Care of Xi’an Jiaotong University. The ‘Principles of Laboratory Animal Care’ (NIH Publication Vol 25, No. 28 revised 1996; http://grants.nih.gov.ezp-prod1.hul.harvard.edu/grants/guide/notice-files/not96-208.htmL) as well as the current version of the Chinese Law on the Protection of Animals were followed.
Procedure
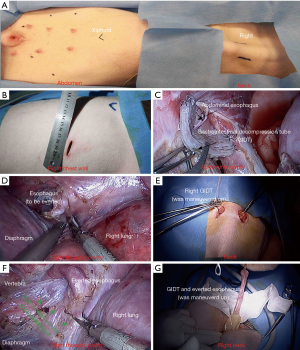
The three pigs each underwent the same procedures: routine laparoscopic techniques, anastomosis of the cervical esophagus with a gastric conduit and thoracoscopic everted esophagectomy. After anesthesia, but prior to the operation, a gastrointestinal decompression tube (GIDT) was placed inside of the stomach. All of the pigs were anesthetized and intubated with a double-lumen endotracheal tube in the conventional manner. A 10 mm thirty-degree scope (Olympus Co.) was used throughout the whole procedure. The ports were shown in Figure 1 (Figure 1A,B). Firstly, we performed the laparoscopic mobilization of the stomach in supine position. The abdominal esophagus and GIDT were simultaneously transected using the endoscopic linear cutter stapler (Johnson & Johnson, Figure 1C). The 30–40 mm gastric conduit was formed from the pylorus to the gastric fundus along the lesser curvature of the stomach using the endoscopic linear cutter staplers (Johnson & Johnson). The substernal tunnel was made from the xiphoid to the leftmost cervical incision. Secondly, the cervical esophagus was dissected through the leftmost cervical incision. The cervical esophagus and the GIDT were transected at the level of the suprasternal fossa. Then, the distal cervical esophagus and the GIDT were pulled from the leftmost cervical incision to the right through the space between the trachea and spine. The gastric conduit was maneuvered up to the left cervical incision through the substernal tunnel. All wounds in the left of the neck and abdomen were closed after the anastomosis of the cervical esophagus with the gastric conduit. Finally, we performed an everted resection of esophagus in the left lateral decubitus position. The abdominal esophagus was drawn up and everted while the GIDT was maneuvered up into the right cervical incision (Figure 1D,E). High tension was present around the distal esophagus while repositioning the GIDT (Figure 1F). Then, the thoracic esophagus was easily dissected from the esophageal hiatus to the thoracic inlet through just one thoracic operative hole and extracted out of the thoracic cavity via the right cervical incision (Figure 2). After the specimen extraction (Figure 1G) and the suture of the thoracic and cervical wounds, the animals were euthanized with an intravenous injection of 10% potassium chloride (20 mL per animal).

Results
The same uniform operations were conducted on all three of the pigs and were completed without incident. The everted resection of the esophagus was successfully accomplished in the three pigs utilizing one thoracoscopic operative hole.
The overall elapsed time of the operation was 130±39 min (range, 123–201 min). The mean operating time was 61±35 min (range, 23–92 min) for dissecting the stomach and abdominal esophagus. It took 9±4 min (range, 5–13 min) for making the gastric conduit. It took about 12±4.5 min (range 8–17 min) for the esophagogastric anastomosis and then, 41±13.6 min (29–56 min) for the everted esophagectomy. Additionally, the mean estimated blood loss was 22±12.5 mL (range, 10–35 mL) during the dissection of the stomach and abdominal esophagus. Very limited bleeding was observed during the formation of the gastric conduit. The mean estimated blood loss during the esophagogastric anastomosis is 14±6 mL (range, 8–20 mL) and 13±6 mL (range, 5–15 mL) during the everted esophagectomy.
Conclusions
The eversion technique has been widely performed in colorectal resections during the modified Dixon operation (5,6), but not yet in esophagectomy. In this improved and modified procedure, we designed the various steps of the operation compared with those MIE previously reported. The routine steps of a three-hole MIE were: thoracoscopic esophageal dissection followed by laparoscopic gastric mobilization and cervical anastomosis (7). In our study, the thoracoscopic everted esophagectomy was instead performed as the last step following the laparoscopic gastric mobilization and the cervical anastomosis. Furthermore, only one thoracic operative hole was needed for the procedure, which reduced the injury on chest wall.
However, one shortcomings of our study was only three animal models were performed. The animals were not continuously fed to see the survival status and complication after operation for limited conditions. So greater confirmation and validation would be necessary with more animal work and human studies going forward.
Acknowledgments
We thank Dr. Yonghui Liu (Shin-Kong Hospital, Taipei) and Dr. Zhongjie Fu (Boston Children’s Hospital, Boston, MA, U.S.) for English edition. We also thank Meirong Shu and Johnson & Johnson China Ltd for technical help and support.
Funding: This work was supported by the Fundamental Research Funds for the Central University of China (grant No. 08143004 to Yong Zhang) and the Funds for Science and Technology Project of Shaanxi Province of China (grant No. 2014K11-02-03-07 to Yong Zhang).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2016.12.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The experiment was conducted in the Beijing science center of Johnson & Johnson China Ltd. The studies were approved by Animal Care of Xi’an Jiaotong University. The ‘Principles of Laboratory Animal Care’ (NIH Publication Vol 25, No. 28 revised 1996; http://grants.nih.gov.ezp-prod1.hul.harvard.edu/grants/guide/notice-files/not96-208.htmL) as well as the current version of the Chinese Law on the Protection of Animals were followed.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lewis I. The surgical treatment of carcinoma of the oesophagus; with special reference to a new operation for growths of the middle third. Br J Surg 1946;34:18-31. [Crossref] [PubMed]
- McKeown KC. Total three-stage oesophagectomy for cancer of the oesophagus. Br J Surg 1976;63:259-62. [Crossref] [PubMed]
- Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-92. [Crossref] [PubMed]
- Zhang Y, Li S, He H, et al. Minimally invasive everted esophagectomy in pig. Asvide 2017;4:108. Available online: http://www.asvide.com/articles/1416
- Dixon CF. Anterior Resection for Malignant Lesions of the Upper Part of the Rectum and Lower Part of the Sigmoid. Ann Surg 1948;128:425-42. [Crossref] [PubMed]
- Zhuo C, Liang L, Ying M, et al. Laparoscopic Low Anterior Resection and Eversion Technique Combined With a Nondog Ear Anastomosis for Mid- and Distal Rectal Neoplasms: A Preliminary and Feasibility Study. Medicine (Baltimore) 2015;94:e2285 [Crossref] [PubMed]
- Luketich JD, Alvelo-Rivera M, Buenaventura PO, et al. Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg 2003;238:486-94; discussion 494-5. [PubMed]
Cite this article as: Zhang Y, Li S, He H, Ma L, Yang X, Geng D, You J, Fu J. A novel approach for minimally invasive everted esophagectomy in pigs. Video-assist Thorac Surg 2017;2:11.


