Single-port video-assisted thoracoscopic surgery (VATS) excision of paravertebral ganglioneuroma: a case report
Introduction
Benign neurogenic tumours represent most of the paravertebral masses. There is a general recommendation to resect them even in asymptomatic patients, while the tumour is small, to avoid a more complex and morbid later removal of a larger tumour (1).
Video-assisted thoracoscopic surgery (VATS) resection is preferred in such cases (2). There are however still very few reports of single-port VATS resection of paravertebral masses (3,4).
Case presentation
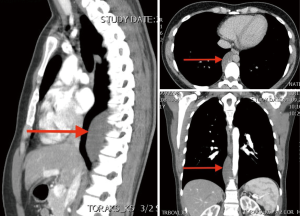
We present a case of a 32-year-old female patient with a 7 cm mass in the right paravertebral space at the level of 8th to 11th thoracic vertebrae (Figure 1). The tumour was discovered incidentally on a CT scan, while running diagnostics for a presumably an ovarian cyst, which turned out to be a teratoma. She was admitted to our department 4 months after removal of the teratoma, without any symptoms, or other physical or laboratory abnormalities.
For the procedure, the patient was placed in a lateral decubitus position. The surgeon and assistant positioned themselves anterior to the patient, with the screen on the opposite side of the patient.
A 3 cm right lateral utility incision was made in the 7th intercostal space in the anterior axillary line. A 10 mm 30-degree high definition (HD) endoscope, was introduced through the anterior part of the incision. During the procedure, all instruments were inserted under the endoscope.
A 2/0 braided nylon suture was first used to retract the diaphragm and obtain perfect visualisation of the tumour. Using a harmonic scalpel, the tumour was carefully dissected and freed from all of the surrounding structures: the azygos vein, aorta and the thoracic duct, which was ligated by two endo-clips. The tumour was extracted using an endobag.
After inflation of the right lung, no chest tube was left in the pleural cavity. The skin was closed using cyanoacrylate skin adhesive. Total duration of the procedure (skin to skin) was 38 minutes (Figure 2).

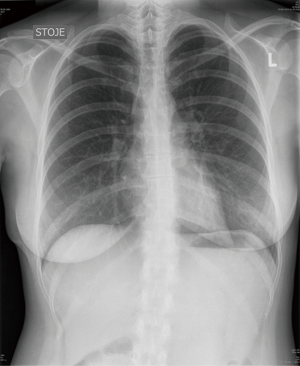
The patient was weaned off the ventilator in the operating theatre and admitted to recovery room for 1 hour. Postoperative recovery was uneventful, the patient was discharged on postoperative day 1. On follow-up visit 2 weeks postoperatively she did not report any symptoms and the CXR was unremarkable (Figure 3).
The pathology report indicated that tumour was a ganglioneuroma (70 mm × 38 mm × 18 mm).
Discussion
In recent years VATS has been widely used for surgical treatment of mediastinal masses. There are however still very few reports of single-port VATS resection of paravertebral masses (3,6). Wu et al. showed that compared to conventional VATS, single-port VATS resection of mediastinal tumours is a promising and safe technique, maybe with a shorter duration, shorter postoperative hospital stay and lower first day postoperative pain score (3).
In the reported case the main difficulty to a VATS resection presented the relatively large size of the tumour and its location very low in the chest, almost at the level of the diaphragm. To obtain an optimal angle for thoracoscopic resection we have approached the tumour through an incision in the 7th intercostal space in the anterior axillary line instead of the usual 4th or 5th. Although in this situation the view of the tumour was almost entirely obstructed by the diaphragm, a perfect view was easily obtained by retracting the diaphragm using a single stitch, pulled out through the anterior part of the incision.
A harmonic scalpel was then used to precisely dissect the surrounding structures such as the azygos vein, aorta and the intercostal branches away from the tumour. Thoracic duct was identified and ligated to prevent complications related to possible chyle leak.
To minimise the invasiveness of the procedure and achieve maximal cosmetic effect, no tube was left in the chest after the expansion of the right lung. The skin was closed using cyanoacrylate skin adhesive.
Conclusions
For an experienced surgeon a single-port approach to the paravertebral tumours does not add any significant technical problems in comparison to conventional VATS.
In this particular case a further reduction of invasiveness could be achieved by performing a tubeless VATS procedure using non-intubated intravenous anaesthesia (7).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2016.10.06). Dr. Stupnik reports personal fees and non-financial support from Johnson & Johnson, outside the submitted work. Dr. Domjan has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Eckardt J, Licht PB. When should large benign tumours in posterior mediastinum be resected? J Thorac Dis 2013;5:E28-30. [PubMed]
- Li Y, Wang J. Experience of video-assisted thoracoscopic resection for posterior mediastinal neurogenic tumours: a retrospective analysis of 58 patients. ANZ J Surg 2013;83:664-8. [Crossref] [PubMed]
- Wu CF, Gonzalez-Rivas D, Wen CT, et al. Comparative Short-Term Clinical Outcomes of Mediastinum Tumor Excision Performed by Conventional VATS and Single-Port VATS: Is It Worthwhile? Medicine (Baltimore) 2015;94:e1975 [Crossref] [PubMed]
- Wu CY, Heish MJ, Wu CF. Single port VATS mediastinal tumor resection: Taiwan experience. Ann Cardiothorac Surg 2016;5:107-11. [Crossref] [PubMed]
- Domjan M, Štupnik T. Single-port video-assisted thoracoscopic (VATS) excison of paravertebral ganglioneuroma. Asvide 2016;3:454. Available online: http://www.asvide.com/articles/1230
- Yim AP. Video-assisted thoracoscopic resection of anterior mediastinal masses. Int Surg 1996;81:350-3. [PubMed]
- Cui F, Liu J, Li S, et al. Tubeless video-assisted thoracoscopic surgery (VATS) under non-intubated, intravenous anesthesia with spontaneous ventilation and no placement of chest tube postoperatively. J Thorac Dis 2016;8:2226-32. [Crossref] [PubMed]
Cite this article as: Domjan M, Štupnik T. Single-port video-assisted thoracoscopic surgery (VATS) excision of paravertebral ganglioneuroma: a case report. Video-assist Thorac Surg 2016;1:33.