Thoracoscopic S6 segmentectomy: tricks to know
Thoracoscopic S6 segmentectomy is seen as one the most straightforward sublobar resection and is frequently the one to start with when experience with thoracoscopic sublobar resections (TSLR) is still limited. However, there are many variations in the anatomy that can make the procedure more difficult than expected. In addition, unusual technical difficulties can be faced and may lead to pitfalls. The aim of this article is to illustrate variations and suggest tips to overcome some technical issues.
This article is based on an experience of 68 S6 segmentectomies, 40 on left and 28 on right side out of a series of 272 thoracoscopic sublobar resections (TSLR). In 2 cases, the S6 segmentectomy was extended to S2 and to S10. Indication was a proven or suspected cT1aN0 non-small cell lung carcinoma (NSCLC) in 48, suspected metastasis in 11 and benign lesion in 9 patients. There were 4 conversions into thoracotomy (5.9%), in one case because the target nodule could not be found and in 3 cases because of a vascular tear that could not be managed thoracoscopically. Mean operative time was 137 min (range: 50–240 min) and mean intraoperative blood loss was 82 cc (range: 0–700 cc). Mean drainage duration and mean hospital stay were 2.6 days (range: 1–8 days) and 4.8 days (range: 2–10 days) respectively. The basics of the technique have been previously reported (1,2) and will not be detailed here, as our aim is only stressing difficulties that can be encountered whatever the approach and technique used. Helpful anatomical description can be found in the atlas of H. Nomori and M. Okada (3).
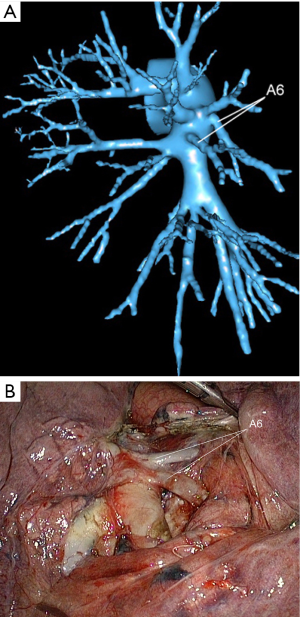
Arteries: variations
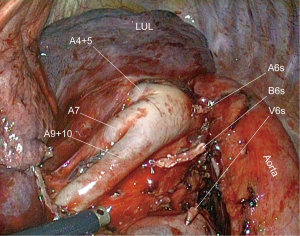
The superior segment of the left lower lobe is supplied by a single (80%) (Figure 1) or double (18%) (Figure 2) or even triple (2%) artery that originates from the posterior aspect of the pulmonary artery in the posterior portion of the fissure. When single, A6 artery bifurcates in 2 or 3 branches. In case of double or triple artery, the main concern is deciding which branches are for segment 6. This is why, even though this segmentectomy is taken to be easy, a preoperative modelisation is helpful.
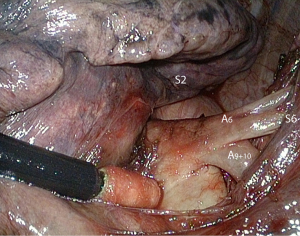
Tributaries to segments S9 and S10 can be close to A6 and must not be confused for an A6 branch (Figure 3).
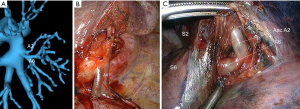
A6 and ascending A2 can arise as a single trunk (Figure 4). Identifying A6 and the origin of A2 before stapling the posterior part of the fissure is important to avoid tearing A2.
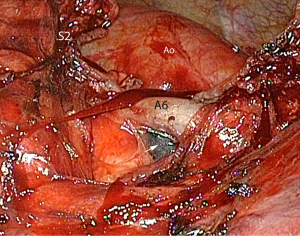
A lymph node is frequently encountered close to the posterior aspect of A6 (Figure 5). It can tightly adhere to the artery and exposes to a vascular tear during dissection.
Veins: variations
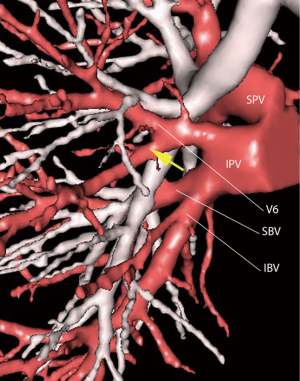
The vein to the superior segment is the uppermost and smaller segmental tributary (V6) of the inferior pulmonary vein (Figure 6). It can usually be divided without problem, but in some cases, V6 can receive a tributary from the basilar segments (Figure 7). In this case, only the uppermost tributary of V6 must be clipped (Figure 8).


Bronchus: variations and unusual situations
The superior segmental bronchus for the lower lobe originates opposite or slightly above the middle lobe or lingular bronchus. It lies posteriorly to the segmental artery. It is single in most patients but can rarely arise as two separate bronchi.
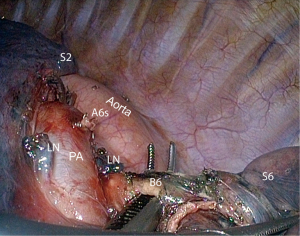
In obese or in some kyphotic patients, the bronchus is located deeply and remote from A6 (Figure 9) so that its identification and dissection can be difficult, especially when dissection is conducted from the front. In these cases, it can be advisable to approach B6 from the back and from below, after division of V6 (Figure 10).
The bronchus is usually thin and can be stapled with a 30 mm endostapler loaded with 3 mm staples. However, when the tumor is at the origin of the bronchus, manual cutting and hand suturing can be necessary (Figure 11).
Fissure division: dealing with a fused fissure
In order to have a precise visualization of the arterial pattern, we favour a fissure first dissection. Only the posterior portion of the fissure needs to be opened.
When the posterior portion of the fissure is absent or loose completing the division can be easily achieved with a vessel sealing device (Figure 12).
However, when the fissure is fused, this can be tricky and we suggest proceeding this way (Figure 13).
Once the pulmonary artery has been identified, a dissecting forceps is introduced from the posterior surface of the artery toward the posterior mediastinum. This may require retracting the lobes forward in order to expose the posterior mediastinal pleura. The pleura is incised at the level of the intermediate bronchus. An oblique viewing endoscope or a deflectable scope is helpful to control this maneuver. The posterior fissure is then stapled.
If the fissure is both thick and long, exposing the posterior mediastinum and the esophagus is usually impossible. It is advisable to shorten the fissure by stapling its most peripheral part. This facilitates retraction of the lobes and exposure of the posterior mediastinum (Figure 11).
Intersegmental plane
A long clamp is applied on the parenchyma, checking that the bronchial stump keeps remote and will not get stuck within the stapler jaws. A reventilation test allows identification of the intersegmental plane. The parenchyma is compressed by the clamp to ease stapler application (Figures 14,15) (9).

Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: One of the authors (DG) is consultant for an instrumentation manufacturer (Delacroix Chevalier). The other authors have no conflict of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from all patients and is available for review by Editors-in Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gossot D, Zaimi R, Fournel L, et al. Totally thoracoscopic pulmonary anatomic segmentectomies: technical considerations. J Thorac Dis 2013;5:S200-6. [PubMed]
- Gossot D. Atlas of endoscopic major pulmonary resections. Paris: Springer-Verlag Paris. 2010.
- Nomori H, Okada M. Illustrated Anatomical Segmentectomy for Lung Cancer. Tokyo: Springer Japan. 2012.
- Seguin-Givelet A, Lutz J, Gossot D. Control of V6 artery. Asvide 2016;3:390. Available online: http://www.asvide.com/articles/1160
- Seguin-Givelet A, Lutz J, Gossot D. Demonstration that after division of V6, the bronchus can be exposed from below (left side). Asvide 2016;3:391. Available online: http://www.asvide.com/articles/1161
- Seguin-Givelet A, Lutz J, Gossot D. Manual division of B6 bronchus for a carcinoid tumor at the origin of the bronchus. In this case, the bronchus is cut back because of an invaded margin at frozen section (right side). Asvide 2016;3:392. Available online: http://www.asvide.com/articles/1162
- Seguin-Givelet A, Lutz J, Gossot D. Division of the posterior portion of a thin fissure (left side). Asvide 2016;3:393. Available online: http://www.asvide.com/articles/1163
- Seguin-Givelet A, Lutz J, Gossot D. Division of the posterior portion of a thick fissure (right side). Asvide 2016;3:394. Available online: http://www.asvide.com/articles/1164
- Ojanguren A, Gossot D, Seguin-Givelet A. Division of the intersegmental plane during thoracoscopic segmentectomy: is stapling an issue? J Thorac Dis 2016;8:2158-64. [Crossref] [PubMed]
Cite this article as: Seguin-Givelet A, Lutz J, Gossot D. Thoracoscopic S6 segmentectomy: tricks to know. Video-assist Thorac Surg 2016;1:24.