
Multiportal vs. uniportal video-assisted thoracoscopic lobectomy: a critical overview
The advent of uniportal video-assisted thoracoscopic lobectomy (uniportal VATS lobectomy) has enlivened the worldwide thoracic surgery community over the last five years. This approach promised the least access trauma of any VATS lobectomy technique thus far (1), but it is striking that the promoters of this technique have not endeavoured sufficiently to prove its hypothetical advantage.
Nevertheless, one should bear in mind that absolute scientific rigour is always a must, hence uniportal VATS has received increasing criticism from some well-respected voices (2-5). Opponents of the uniportal approach point out the technical challenge of having all instrumentation sharing the same access incision alongside the thoracoscope (4,6). Simultaneous insertion of the scope and instruments, it is argued, leads undoubtedly to compromised dexterity and patient safety; adequacy of oncologic clearance could be not reached either (3,4).
When multi portal video-assisted thoracoscopic lobectomy (multi portal VATS lobectomy) was first developed in the 1990s, it represented as much of a technical revolution then as uniportal VATS does now. Of course, innovation through changing the standards of surgical practice, is not only acceptable but should also be the aim of professional associations and individuals, but doing so requires scientific evidence, gained from well-designed studies.
What is the evidence for uniportal VATS?
It is my contention that an adequate number of case reports and simple case series (7,8) on this approach have been published over the last few years. Future papers from a single institute’s experience in performing uniportal VATS lobectomy may actually be considered as irrelevant because the point related to proving the safety and feasibility of this approach has already been demonstrated: there are no reports in published literature to show that this technique is harmful.
In contrast, a very few number of comparative studies are present in published literature. Let us focus on the most recent of them: one from 2013 (9), eight from 2015 (10-17) and two from 2016 (18,19). A summary of the aforementioned is provided in Table 1.
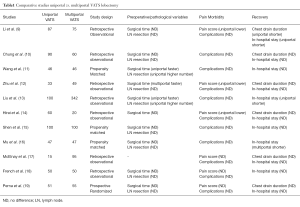
Full table
Interestingly, eight of these studies originated from Asia, two from Europe (United Kingdom and Spain) and only one from North America (Canada). Of the eleven studies, seven were unmatched comparisons, three were case-matched studies and only one was a prospective randomized study. All studies focused on preoperative-pathological variables (except McElnay et al.) and on postoperative clinical outcomes. Only one study compared the 30-day mortality rate and none of them mentioned the medium-long term follow-up or overall cancer related survival rates.
Main findings
- Preoperative-pathological variables: Zhu et al. (12) pointed out that multiportal is faster than uniportal VATS. Only two studies from the same centre (11,13) concluded that uniportal VATS had a shorter operation time and a major number of lymph node resections. None of the remaining eight studies showed differences concerning these variables;
- Postoperative clinical outcomes: only three studies showed differences in postoperative pain score in favour of uniportal VATS (9,12,14) but not concerning complications. It is relevant to point out that in two of these three studies (12,14) there is no evidence that intraoperative analgesia or postoperative analgesia had been standardized amongst all patients. The remaining eight studies did not show differences in pain and complications.
- Recovery: Liu et al. (13) pointed out that the uniportal VATS group had a shorter in-hospital stay; instead, according to Mu et al. (16) it was the uniportal group that showed a larger in-hospital stay because of the poorer wound healing at the chest drain site. Li et al. (9) observed that uniportal VATS had a shorter chest drain duration and a shorter in-hospital stay. The remaining eight studies did not show any differences in chest drain duration and in-hospital stay.
Harris et al. (20) published in 2016 a systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. The author stated that: “Electronic searches were performed using Ovid Medline, Embase, PubMed, the Cochrane Database of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR), ACP Journal Club and Database of Abstracts of Reviews of Effects (DARE) from their inception date to January 2016”. After applying the selection criteria and excluding the studies that compared uniportal and multiportal VATS for indications other than lung cancer, eight studies remained for assessment. It is interesting to note that all these studies are the same we have discussed and summarized in Table 1, except for McElnay’s (17) one, though it was published in 2015. Harris concluded that uniportal VATS was associated with a statistically significant shorter duration of chest tube drainage, shorter in-hospital stay and lower overall morbidity compared with multiportal VATS; instead, when propensity data were analysed, there were no statistically significant differences in operation time, length of hospital stay, duration of postoperative drainage and overall morbidity.
Ultimately, what kind of conclusions can be drawn following this thorough analysis of published scientific literature?
Is there a need to generate more and better clinical data to define the role of uniportal VATS?
Maybe there is, given that of the eleven cited comparative studies, seven were unmatched comparisons, three were case-matched studies and only one was a prospective randomized study. The latter (19) represents the sole prospective randomized study published so far and the only one that compared the 30-day mortality rate. Perna et al. had already stressed the importance of the starting points for future studies:
- Sample size estimation is mandatory to minimize bias;
- The most important measure of treatment efficacy when it comes to lung cancer must be survival; it is clear that data about mid-long term follow-up and cancer overall survival are still needed.
At the time of this writing, one could honestly draw these conclusions:
- Uniportal VATS is safe and feasible and only those who have mastered the necessary skills should perform it;
- There is no evidence that uniportal VATS is related to better postoperative outcomes when compared with multiportal VATS.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Video-Assisted Thoracic Surgery. The article did not undergo external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/vats.2016.08.07). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Sihoe AD. Reasons not to perform uniportal VATS lobectomy. J Thorac Dis 2016;8:S333-43. [PubMed]
- 23rd European Conference on General Thoracic Surgery, Lisbon Portugal. 23rd European Conference on General Thoracic Surgery, Lisbon, Portugal. 2015.
- Van Raemdonck D, Sihoe AD. Postgraduate symposium on general thoracic surgery. Lisbon, Portugal: the European Society of Thoracic Surgeons at the 23rd European Conference on General Thoracic Surgery; May 31, 2015.
- Hansen HJ. VATS lobectomy: multiport access is the optimal access. Lisbon, Portugal: Breakfast Session conducted by the European Society of Thoracic Surgeons at the 23rd European Conference on General Thoracic Surgery; June 2, 2015.
- Bertolaccini L, Viti A, Terzi A. Ergon-trial: ergonomic evaluation of single-port access versus three-port access video-assisted thoracic surgery. Surg Endosc 2015;29:2934-40. [Crossref] [PubMed]
- Feng M, Shen Y, Wang H, et al. Uniportal video assisted thoracoscopic lobectomy: primary experience from an Eastern center. J Thorac Dis 2014;6:1751-6. [PubMed]
- Ismail M, Helmig M, Swierzy M, et al. Uniportal VATS: the first German experience. J Thorac Dis 2014;6:S650-5. [PubMed]
- Li C, Ma H, He J, et al. Clinical analysis of thoracoscopic lobectomy in the treatment of peripheral lung cancer with single utility port. Zhongguo Fei Ai Za Zhi 2013;16:487-91. [PubMed]
- Chung JH, Choi YS, Cho JH, et al. Uniportal video-assisted thoracoscopic lobectomy: an alternative to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015;20:813-9. [Crossref] [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [Crossref] [PubMed]
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [PubMed]
- Liu CC, Shih CS, Pennarun N, et al. Transition from a multiport technique to a single-port technique for lung cancer surgery: is lymph node dissection inferior using the single-port technique?†. Eur J Cardiothorac Surg 2016;49:i64-72. [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes†. Eur J Cardiothorac Surg 2016;49:i37-41. [PubMed]
- Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study†. Eur J Cardiothorac Surg 2016;49:i48-53. [PubMed]
- Mu JW, Gao SG, Xue Q, et al. A Matched Comparison Study of Uniportal Versus Triportal Thoracoscopic Lobectomy and Sublobectomy for Early-stage Nonsmall Cell Lung Cancer. Chin Med J (Engl) 2015;128:2731-5. [Crossref] [PubMed]
- McElnay PJ, Molyneux M, Krishnadas R, et al. Pain and recovery are comparable after either uniportal or multiport video-assisted thoracoscopic lobectomy: an observation study. Eur J Cardiothorac Surg 2015;47:912-5. [Crossref] [PubMed]
- French DG, Thompson C, Gilbert S, et al. Transition from multiple port to single port video-assisted thoracoscopic anatomic pulmonary resection: early experience and comparison of perioperative outcomes. Ann Cardiothorac Surg 2016;5:92-9. [Crossref] [PubMed]
- Perna V, Carvajal AF, Torrecilla JA, et al. Uniportal video-assisted thoracoscopic lobectomy versus other video-assisted thoracoscopic lobectomy techniques: a randomized study. Eur J Cardiothorac Surg 2016; [Epub ahead of print]. [Crossref] [PubMed]
- Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg 2016;5:76-84. [Crossref] [PubMed]
Cite this article as: Perna V. Multiportal vs. uniportal video-assisted thoracoscopic lobectomy: a critical overview. Video-assist Thorac Surg 2016;1:19.


